Validity and reliability of neonatal infant pain scale (NIPS) in neonatal intensive care unit in Viet Nam
The study aimed to culturally adapt and validate Neonatal Infant Pain Scale (NIPS)
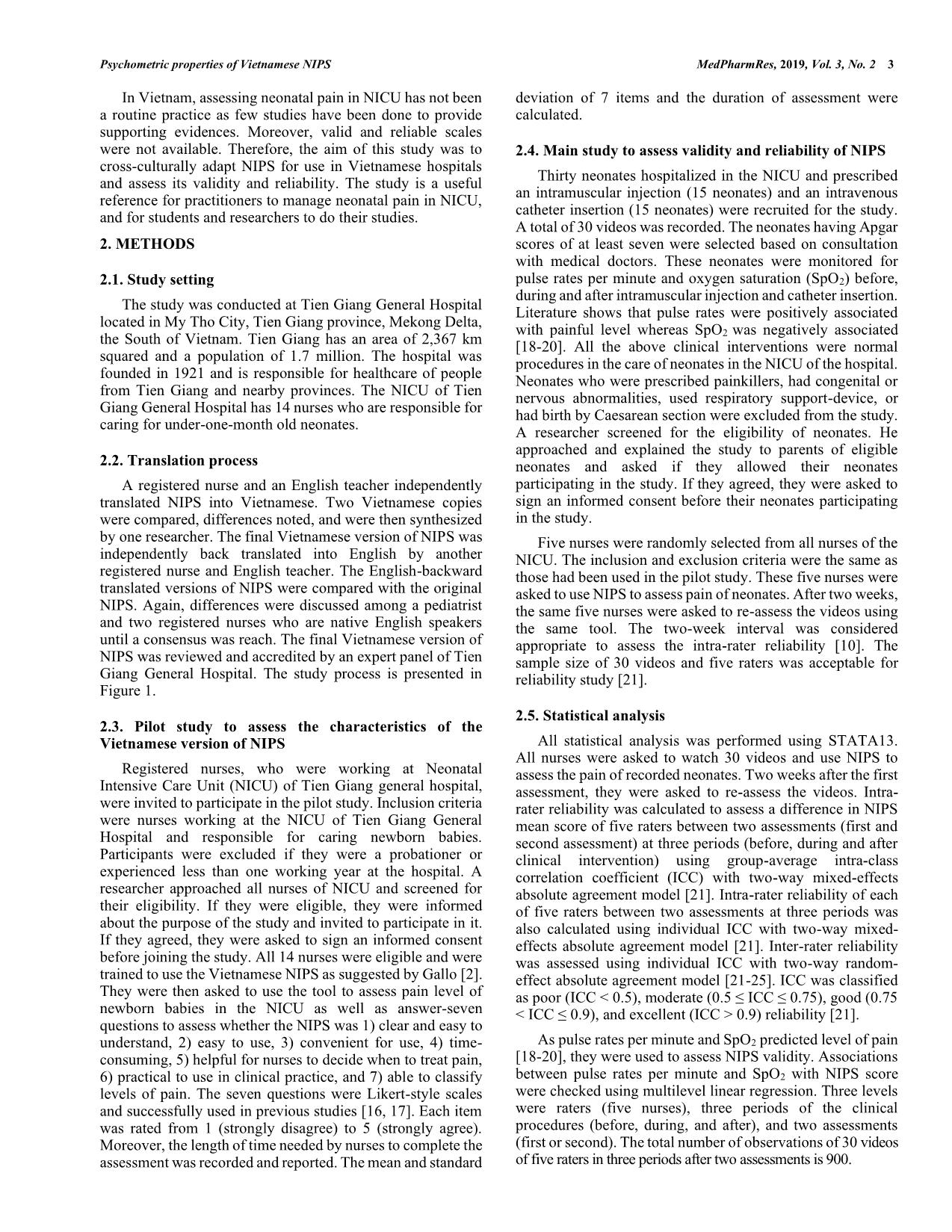
for use in Vietnamese settings. Methods: The original NIPS was translated into Vietnamese using a standard
protocol. Registered nurses of Neonatal Intensive Care Unit (NICU), Tien Giang General Hospital, Vietnam
used the Vietnamese NIPS for assessing neonatal pain and then provided feedback on acceptability of the scale.
Five registered nurses of NICU were randomly selected and used NIPS for assessing neonatal pain while
watching thirty videos at two times, two weeks apart from each other. Pulse rates per minute and oxygen
saturation (SpO2) were also recorded for validity evaluation. Intraclass correlation coefficients (ICC) with twoway random effects were applied to assess intra-rater and inter-rater reliability. Multilevel linear regression was
applied to assess the association between NIPS score with pulse rates and SpO2 adjusting for raters, three
periods and two assessments. Results: The Vietnamese NIPS was accepted and valued by nurses at the NICU.
ICCs between the first and second assessments were from 0.53 to 1.00 for five raters before, during and after
clinical procedures showing moderate to excellent intra-rater reliability. ICCs among five raters were moderate
to good before and after, but poor (ICC<0.4) during clinical procedures. NIPS score was not associated with
SpO2, but with pulse rates per minute. Conclusions: The preliminary results showed that the Vietnamese
version of NIPS is reliable and should be used. However, it is recommended that further research should be
conducted to confirm its reliability and validity.
Trang 1
Trang 2
Trang 3
Trang 4
Trang 5

Trang 6
Trang 7
Tóm tắt nội dung tài liệu: Validity and reliability of neonatal infant pain scale (NIPS) in neonatal intensive care unit in Viet Nam

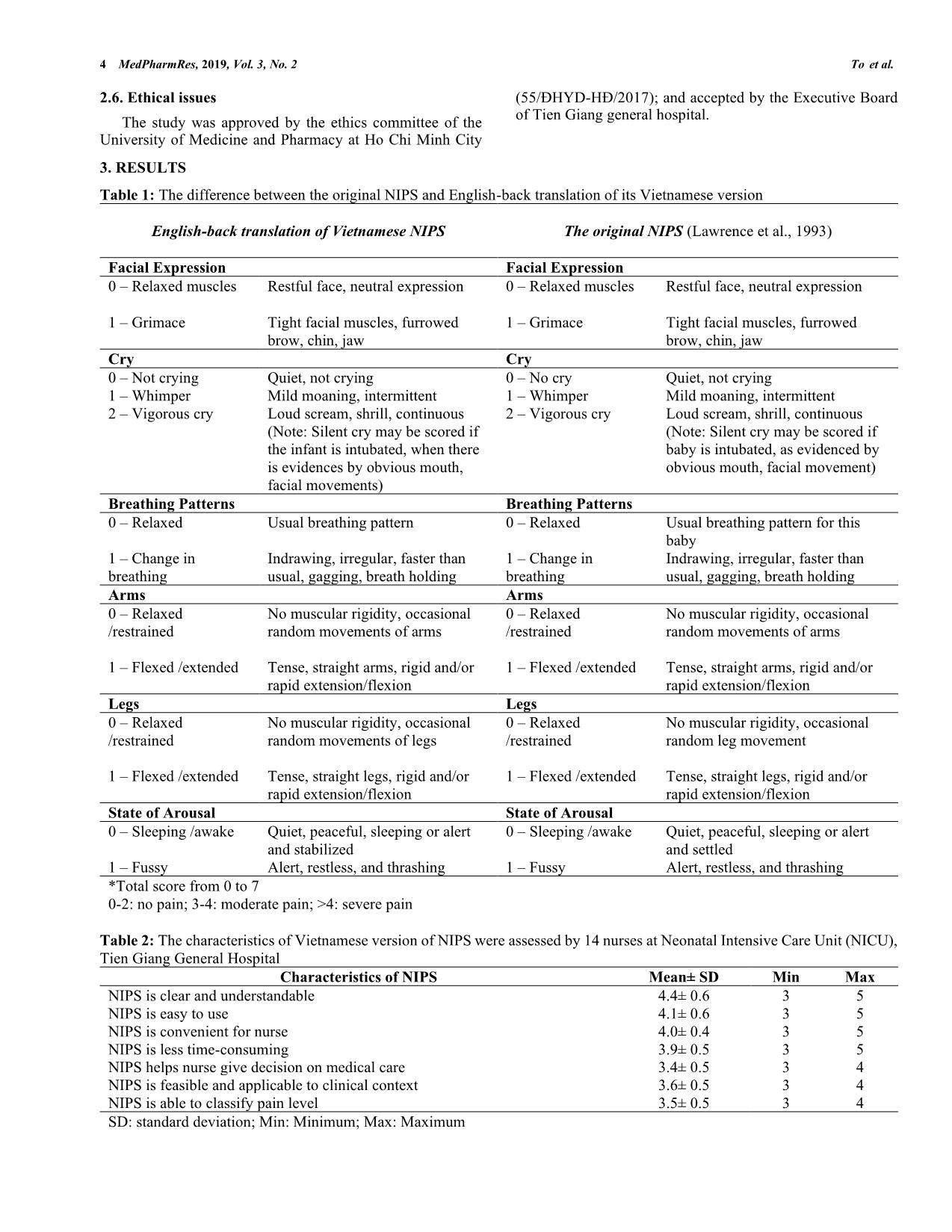
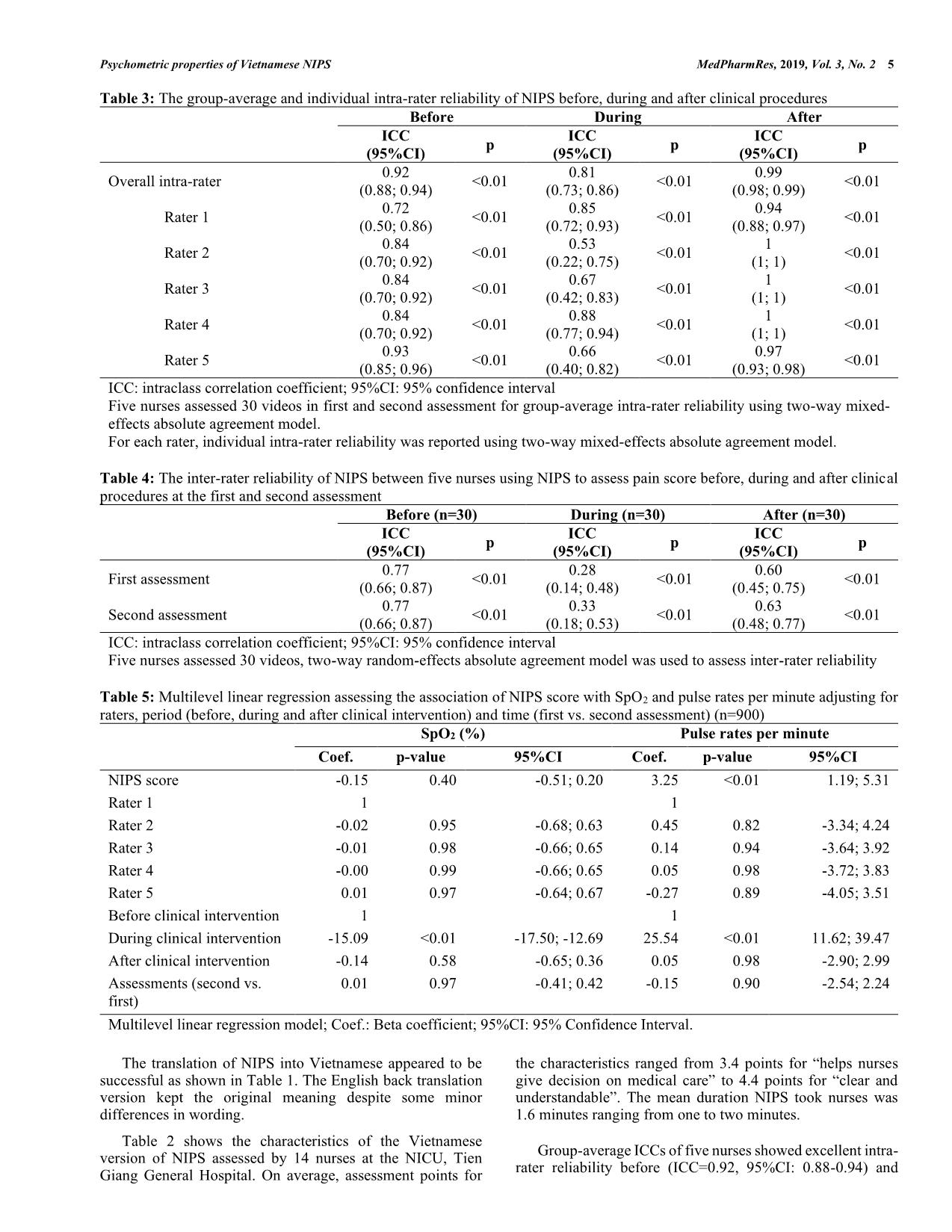
MedPharmRes, 2019, 3 1 *Address correspondence to Kien Gia To at the Faculty of Public Health, University of Medicine and Pharmacy at Ho Chi Minh City; 217 Hong Bang, Ward 11, District 5, Ho Chi Minh City, Vietnam; Tel/Fax: (+84) 91 95 11 121; E-mails: kiengiato@gmail.com or togiakien@ump.edu.vn DOI: 10.32895/UMP.MPR.3.2.1 © 2019 MedPharmRes MedPharmRes journal of University of Medicine and Pharmacy at Ho Chi Minh City homepage: and Original article Validity and Reliability of Neonatal Infant Pain Scale (NIPS) in Neonatal Intensive Care Unit in Vietnam Hai Thanh Ngoa, Kathleen Fitzsimmonsb, Kien Gia Toc* aVINMEC General Hospital; 208 Nguyen Huu Canh, Ward 22, Binh Thanh District, Ho Chi Minh City, Vietnam; bGreenville County Schools, Greenville, South Carolina, USA; cFaculty of Public Health, University of Medicine and Pharmacy at Ho Chi Minh City; 217 Hong Bang, Ward 11, District 5, Ho Chi Minh City, Vietnam. Received July 14, 2018: Revised June 11, 2019: Accepted July 04, 2019 Abstract: Background: The study aimed to culturally adapt and validate Neonatal Infant Pain Scale (NIPS) for use in Vietnamese settings. Methods: The original NIPS was translated into Vietnamese using a standard protocol. Registered nurses of Neonatal Intensive Care Unit (NICU), Tien Giang General Hospital, Vietnam used the Vietnamese NIPS for assessing neonatal pain and then provided feedback on acceptability of the scale. Five registered nurses of NICU were randomly selected and used NIPS for assessing neonatal pain while watching thirty videos at two times, two weeks apart from each other. Pulse rates per minute and oxygen saturation (SpO2) were also recorded for validity evaluation. Intraclass correlation coefficients (ICC) with two- way random effects were applied to assess intra-rater and inter-rater reliability. Multilevel linear regression was applied to assess the association between NIPS score with pulse rates and SpO2 adjusting for raters, three periods and two assessments. Results: The Vietnamese NIPS was accepted and valued by nurses at the NICU. ICCs between the first and second assessments were from 0.53 to 1.00 for five raters before, during and after clinical procedures showing moderate to excellent intra-rater reliability. ICCs among five raters were moderate to good before and after, but poor (ICC<0.4) during clinical procedures. NIPS score was not associated with SpO2, but with pulse rates per minute. Conclusions: The preliminary results showed that the Vietnamese version of NIPS is reliable and should be used. However, it is recommended that further research should be conducted to confirm its reliability and validity. Keywords: NIPS, reliability, validity, NICU, Vietnam. 1. INTRODUCTION Pain is defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” [1]. Pain in neonates has been extensively studied in recent years and evidence suggests that neonates experience pain much more severe than adult or older children do as neonatal pain seriously affects development of nervous system and growing of babies [2]. Literatures showed that neonates experience many painful and stressful procedures in Neonatal Intensive Care Unit (NICU) [3-5]. Pain should be assessed for optimal care of neonates in NICU [5, 6]; however, assessing pain is very difficult and complicated, particularly in neonates as they are unable to verbally communicate [5, 7]. Although some validated and reliable pain scales are available for assessing neonatal pain, 2 MedPharmRes, 2019, Vol. 3, No. 2 To et al. they are rarely used in clinical practice and most of the scales are in English which require translation and cross-cultural adaptation for use in local contexts [4, 5, 8-11]. Neonatal Infant Pain Scale (NIPS) was developed by Lawrence et al. at Children’s Hospital of Eastern Ontario to assess pain in neonates based on behaviors. Their study included videotaping 90 medical procedures of 38 neonates before, during and after procedures [12]. The Cronbach’s Alpha coefficients before, during and after procedures were 0.95, 0.87 and 0.88, respectively. The Pearson correlation was 0.92 to 0.97 showed good inter-rater reliability. NIPS includes six items assessing six states of neonates including facial expression, cry, breathing patterns, movement of arms, movement of legs and state of arousal. Each item is scored 0 to 1, except state of cry is scored 0, 1 and 2, for a possible total score of 7. Neonates have no pain if NIPS score is 0-2, moderate pain if NIPS score is 3-4 and severe pain if NIPS score is more than 4. NIPS has the advantage that it does not require users have additional skills or equipment to assess pain and would be a good tool for assessing and improving pain management of neonates [2, 4]. Moreover, ... armRes, 2019, Vol. 3, No. 2 5 Table 3: The group-average and individual intra-rater reliability of NIPS before, during and after clinical procedures Before During After ICC (95%CI) p ICC (95%CI) p ICC (95%CI) p Overall intra-rater 0.92 (0.88; 0.94) <0.01 0.81 (0.73; 0.86) <0.01 0.99 (0.98; 0.99) <0.01 Rater 1 0.72 (0.50; 0.86) <0.01 0.85 (0.72; 0.93) <0.01 0.94 (0.88; 0.97) <0.01 Rater 2 0.84 (0.70; 0.92) <0.01 0.53 (0.22; 0.75) <0.01 1 (1; 1) <0.01 Rater 3 0.84 (0.70; 0.92) <0.01 0.67 (0.42; 0.83) <0.01 1 (1; 1) <0.01 Rater 4 0.84 (0.70; 0.92) <0.01 0.88 (0.77; 0.94) <0.01 1 (1; 1) <0.01 Rater 5 0.93 (0.85; 0.96) <0.01 0.66 (0.40; 0.82) <0.01 0.97 (0.93; 0.98) <0.01 ICC: intraclass correlation coefficient; 95%CI: 95% confidence interval Five nurses assessed 30 videos in first and second assessment for group-average intra-rater reliability using two-way mixed- effects absolute agreement model. For each rater, individual intra-rater reliability was reported using two-way mixed-effects absolute agreement model. Table 4: The inter-rater reliability of NIPS between five nurses using NIPS to assess pain score before, during and after clinical procedures at the first and second assessment Before (n=30) During (n=30) After (n=30) ICC (95%CI) p ICC (95%CI) p ICC (95%CI) p First assessment 0.77 (0.66; 0.87) <0.01 0.28 (0.14; 0.48) <0.01 0.60 (0.45; 0.75) <0.01 Second assessment 0.77 (0.66; 0.87) <0.01 0.33 (0.18; 0.53) <0.01 0.63 (0.48; 0.77) <0.01 ICC: intraclass correlation coefficient; 95%CI: 95% confidence interval Five nurses assessed 30 videos, two-way random-effects absolute agreement model was used to assess inter-rater reliability Table 5: Multilevel linear regression assessing the association of NIPS score with SpO2 and pulse rates per minute adjusting for raters, period (before, during and after clinical intervention) and time (first vs. second assessment) (n=900) SpO2 (%) Pulse rates per minute Coef. p-value 95%CI Coef. p-value 95%CI NIPS score -0.15 0.40 -0.51; 0.20 3.25 <0.01 1.19; 5.31 Rater 1 1 1 Rater 2 -0.02 0.95 -0.68; 0.63 0.45 0.82 -3.34; 4.24 Rater 3 -0.01 0.98 -0.66; 0.65 0.14 0.94 -3.64; 3.92 Rater 4 -0.00 0.99 -0.66; 0.65 0.05 0.98 -3.72; 3.83 Rater 5 0.01 0.97 -0.64; 0.67 -0.27 0.89 -4.05; 3.51 Before clinical intervention 1 1 During clinical intervention -15.09 <0.01 -17.50; -12.69 25.54 <0.01 11.62; 39.47 After clinical intervention -0.14 0.58 -0.65; 0.36 0.05 0.98 -2.90; 2.99 Assessments (second vs. first) 0.01 0.97 -0.41; 0.42 -0.15 0.90 -2.54; 2.24 Multilevel linear regression model; Coef.: Beta coefficient; 95%CI: 95% Confidence Interval. The translation of NIPS into Vietnamese appeared to be successful as shown in Table 1. The English back translation version kept the original meaning despite some minor differences in wording. Table 2 shows the characteristics of the Vietnamese version of NIPS assessed by 14 nurses at the NICU, Tien Giang General Hospital. On average, assessment points for the characteristics ranged from 3.4 points for “helps nurses give decision on medical care” to 4.4 points for “clear and understandable”. The mean duration NIPS took nurses was 1.6 minutes ranging from one to two minutes. Group-average ICCs of five nurses showed excellent intra- rater reliability before (ICC=0.92, 95%CI: 0.88-0.94) and 6 MedPharmRes, 2019, Vol. 3, No. 2 To et al. after (ICC=0.99, 95%CI: 0.98-0.99) clinical procedures, but good (ICC=0.81, 95%CI: 0.73-0.86) during clinical procedure (p<0.01) (table 3). All individual ICCs showed good to excellent agreements (ICC ≥ 0.84) with the exception of rater 1 before clinical procedures, and rater 2, 3, 5 during clinical procedure just showing moderate agreement (ICC=0.53 to 0.72, p<0.01). At first and second assessments, almost 100% videos were rated no pain before clinical procedure at the first and second assessments. Five nurses showed good agreements (ICC=0.77, 95%CI: 0.66-0.87) before clinical procedures, poor agreements (ICC=0.28, 95%CI: 0.14-0.48 and 0.33, 95%CI: 0.18-0.53) during clinical procedures, and moderate agreements (ICC=0.60, 95%CI: 0.45-0.75 and 0.63, 95%CI: 0.48-0.77) after clinical procedures (p<0.01) at the first and second assessments (table 4). After adjusting for raters, periods and assessments, the multilevel linear regression showed that NIPS score was not significantly associated with SpO2 (p>0.05). However, for every point increase in NIPS score, pulse rate per minute increased three beats (p<0.01) (Table 5). 4. DISCUSSION This study translated and adapted the original NIPS into Vietnamese using the process guided by World Health Organization [26]. English-Vietnamese and Vietnamese-English translations of NIPS is highly consistent. The Vietnamese version of NIPS were also reviewed and accredited by experts and experienced NICU nurses. In order to apply the NIPS, it is important that hospitals’ nurses accept and are willing to use it. Our study indicated that all nurses agreed that the Vietnamese version of NIPS is applicable in the local hospital context. The NIPS mean score indicated that neonates have almost no pain before and after procedures but severe pain during them. Neonatal pain is highly frequent in NICU because neonates suffered seven invasive procedures per day on average and a half of them had at least pain once during their hospitalization [27]. Compared to other neonatal pain assessment tools, NIPS is easy to use and not time-consuming; and does not require extra equipment [5]. Therefore, NIPS is applicable in NICU. The Vietnamese version of NIPS had good test-retest reliability as its average ICCs of five raters were above 0.75 before, during and after clinical procedures, and individual ICCs were from moderate to excellent (0.53 to 1). Five raters showed good agreements (ICC=0.77) before clinical procedures and moderate agreements (ICC≥0.60) after clinical procedures at first and second assessment. However, poor agreement (ICC<0.4) were detected between the five raters during clinical procedures at the two assessments. As rater 2 had lower ICCs during clinical procedures, this rater was removed from the calculation. ICCs were re-calculated among the other four raters which improved to 0.51 at the first assessment and 0.49 at the second assessment. A possible explanation was that four raters had different level of clinical experiences from the rater 2 as an experienced pediatric nurse tends to rate lower pain score [28]. However, the explanation could not be confirmed as personal data of raters were not collected in this study. More training on how to identify different aspects of pain may be provided to nurses to help increase inter-rater reliability. This study used SpO2 and pulse rates per minute which were objective measures to assess validity of the NIPS. Although the NIPS score was not significantly associated with SpO2, it was positively associated with pulse rates. This finding may reflect the inconsistent results in previous studies. While some showed that heart rate increased and SpO2 decreased during painful procedures [15, 18], the other found that heart rate and SpO2 were not sensitive and not associated with pain scores [29]. Our study has some limitations. Firstly, due to very low variability, it was unable to calculate internal consistency for the entire scale. Secondly, although there are many clinical procedures conducted in the NICU, only two clinical procedures were observed in this study, including intramuscular injection and intravenous catheter insertion. Thirdly, the sample size is small and the study was only conducted in one hospital in the South of Vietnam. Therefore, the results may not be generalizable to other areas of the country. In conclusion, the preliminary results showed that the Vietnamese version of NIPS showed acceptable reliability for use in clinical settings. As there was currently no validated tool for assessing neonatal pain available in Vietnamese, this tool should be used although it is recommended that further research should be conducted to confirm its reliability and validity. LIST OF ABBREVIATIONS ICC: intra-class correlation coefficient; NICU: Neonatal Intensive Care Unit; SpO2: Oxygen saturation. CONFLICT OF INTEREST The authors declare that they have no competing interests. ACKNOWLEDGEMENTS We would like to thank Dr. Quyen Gia To, Queensland University of Technology, for his helpful advice on statistics. Our special thanks should go to nurses of Neonatal Intensive Care Unit and the Executive Board of Tien Giang Hospital for accepting the study. We also thank Dr. Deborah Kupecz for her helpful comments on translation; the reviewers for their useful comments on the manuscript; and all participants for participating in this study. All other contributions to the study should be acknowledged. REFERENCES 1. Loeser JD, Treede RD. The Kyoto protocol of IASP Basic Pain Terminology. Pain. 2008;137(3):473-7. 2. Gallo AM. The fifth vital sign: implementation of the Neonatal Infant Pain Scale. J Obstet Gynecol Neonatal Nurs. 2003;32(2):199-206. 3. Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA. 2008;300(1):60-70. 4. Polkki T, Korhonen A, Axelin A, Saarela T, Laukkala H. Development and preliminary validation of the Neonatal Infant Acute Pain Assessment Scale (NIAPAS). Int J Nurs Stud. 2014;51(12):1585-94. 5. American Academy of Pediatrics. Prevention and management of pain in the neonate: an update. Committee on Fetus and Newborn and Section on Surgery, Section on Anesthesiology and Pain Medicine, Canadian Paediatric Society, and Fetus and Newborn Committee; 2006 Nov. Report No.: 1098-4275 (Electronic), 0031-4005 (Linking) Contract No.: 5. 6. Aukes DI, Roofthooft DW, Simons SH, Tibboe D, van Dijk M. Pain Management in Neonatal Intensive Care: Evaluation of the Compliance with Guidelines. Clin J Pain. 2014. 7. Bhalla T, Shepherd E, Tobias JD. Neonatal pain management. Saudi J Anaesth. 2014;8(Suppl 1):S89-97. Psychometric properties of Vietnamese NIPS MedPharmRes, 2019, Vol. 3, No. 2 7 8. Guedj R, Danan C, Daoud P, Zupan V, Renolleau S, Zana E, et al. Does neonatal pain management in intensive care units differ between night and day? An observational study. BMJ Open. 2014;4(2):e004086. 9. Medicine COFNSOAP. Prevention and Management of Procedural Pain in the Neonate: An Update. Pediatrics. 2016;137(2):e20154271. 10. Motta Gde C, Schardosim JM, Cunha ML. Neonatal Infant Pain Scale: Cross-Cultural Adaptation and Validation in Brazil. J Pain Symptom Manage. 2015;50(3):394-401. 11. Stapelkamp C, Carter B, Gordon J, Watts C. Assessment of acute pain in children: development of evidence-based guidelines. International journal of evidence-based healthcare. 2011;9(1):39-50. 12. Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C. The development of a tool to assess neonatal pain. Neonatal Netw. 1993;12(6):59-66. 13. Hudson-Barr D, Capper-Michel B, Lambert S, Palermo TM, Morbeto K, Lombardo S. Validation of the Pain Assessment in Neonates (PAIN) scale with the Neonatal Infant Pain Scale (NIPS). Neonatal Netw. 2002;21(6):15-21. 14. Malarvizhi G, Manju V, Roseline M, Nithin S, Sarah P. Inter-rater reliability of neonatal infant pain scale (NIPS) as a multidimensional behavioural pain tool. Nitte University Journal of Health Science. 2012;2(1):26-30. 15. Sarhangi F, Mollahadi M, Ebadi A, Matinzadeh ZK, Tadrisi SD. Validity and reliability of Neonatal Infant Pain Scale in Neonatal Intensive Care Units in Iran (2010). Pak J Med Sci. 2011;27(5):1087-91. 16. Suraseranivongse S, Kaosaard R, Intakong P, Pornsiriprasert S, Karnchana Y, Kaopinpruck J, et al. A comparison of postoperative pain scales in neonates. Br J Anaesth. 2006;97(4):540-4. 17. Taddio A, Hogan ME, Moyer P, Girgis A, Gerges S, Wang L, et al. Evaluation of the reliability, validity and practicality of 3 measures of acute pain in infants undergoing immunization injections. Vaccine. 2011;29(7):1390-4. 18. Taksande AM, Vilhekar KY, Jain M, Chitre D. Pain response of neonates to venipuncture. Indian J Pediatr. 2005;72(9):751-3. 19. Gokulu G, Bilgen H, Ozdemir H, Sarioz A, Memisoglu A, Gucuyener K, et al. Comparative heel stick study showed that newborn infants who had undergone repeated painful procedures showed increased short-term pain responses. Acta paediatrica (Oslo, Norway : 1992). 2016;105(11):e520- e5. 20. Porter FL, Wolf CM, Miller JP. Procedural pain in newborn infants: the influence of intensity and development. Pediatrics. 1999;104(1):e13. 21. Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155-63. 22. StataCorp LLC. ICC - Intraclass correlation coefficients [Available from: https://www.stata.com/manuals/ricc.pdf#riccRemarksandexamples. 23. Yoon PJ, Starr JR, Perkins JA, Bloom D, Sie KCY. Interrater and Intrarater Reliability in the Evaluation of Velopharyngeal Insufficiency Within a Single Institution. Archives of Otolaryngology–Head & Neck Surgery. 2006;132(9):947-51. 24. Eliasziw M, Young SL, Woodbury MG, Fryday-Field K. Statistical methodology for the concurrent assessment of interrater and intrarater reliability: using goniometric measurements as an example. Physical therapy. 1994;74(8):777-88. 25. McGraw KO, Wong SP. Forming Inferences About Some Intraclass Correlation Coefficients. Psychological Methods. 1996;1(1):30-46. 26. World Health Organization. Process of translation and adaptation of instruments 2017 [Available from: 27. Sposito NPB, Rossato LM, Bueno M, Kimura AF, Costa T, Guedes DMB. Assessment and management of pain in newborns hospitalized in a Neonatal Intensive Care Unit: a cross-sectional study. Revista Latino- Americana de Enfermagem. 2017;25:e2931. 28. Gomez RJ, Barrowman N, Elia S, Manias E, Royle J, Harrison D. Establishing intra- and inter-rater agreement of the Face, Legs, Activity, Cry, Consolability scale for evaluating pain in toddlers during immunization. Pain research & management. 2013;18(6):e124-e8. 29. Backus LA. Validation of the Neonatal Infant Pain Scale. Michigan, United States: Grand Valley State University; 1996.
File đính kèm:
 validity_and_reliability_of_neonatal_infant_pain_scale_nips.pdf
validity_and_reliability_of_neonatal_infant_pain_scale_nips.pdf

