Knowledge and practice on skin-to-skin contact and early breastfeeding methods of women with vaginal delivery at ha noi obstetrics and gynecology hospital
To describe the knowledge,
practice of skin to skin and early
breastfeeding of women with vaginal
delivery at the Hanoi Obstetrics and
Gynecology Hospital. 2. To examine the
factors related to the practice of skin-toskin and early breastfeeding of women with
vaginal delivery at the Hanoi Obstetrics and
Gynecology Hospital. Method: Postpartum
women at ward A2, Hanoi Obstetrics and
Gynecology Hospital were recruited to the
study. Results: 97% of pregnant women
knew the method of skin-to-skin treatment
for their infants; 81.5% of the women knew
that the benefit of skin-to-skin care is to keep
the baby warm; Only 38.9% of infants were
allowed to skin-to-skin contact with their
mothers in the postpartum room. 79.4% of
pregnant women reported that colostrum is
rich in antibodies, 37.7% of children were
breastfed immediately after skin-to-skin
contact with mother; 19.1% of women were
not supported while breastfeeding the first
meal, 19.1% of the women were assisted
to breastfeed their baby. No relationship
has been found between women ’s age,
education and occupation, and skin-toskin practice and early breastfeeding.
Conclusion: 38.9% of children were skinto-skin contact with their mothers in the
postpartum room; 37.7% of children were
breastfed the immediately after skin-to-skin
contact with their mothers.
Trang 1
Trang 2
Trang 3
Trang 4
Trang 5
Trang 6
Trang 7
Trang 8
Trang 9
Tóm tắt nội dung tài liệu: Knowledge and practice on skin-to-skin contact and early breastfeeding methods of women with vaginal delivery at ha noi obstetrics and gynecology hospital

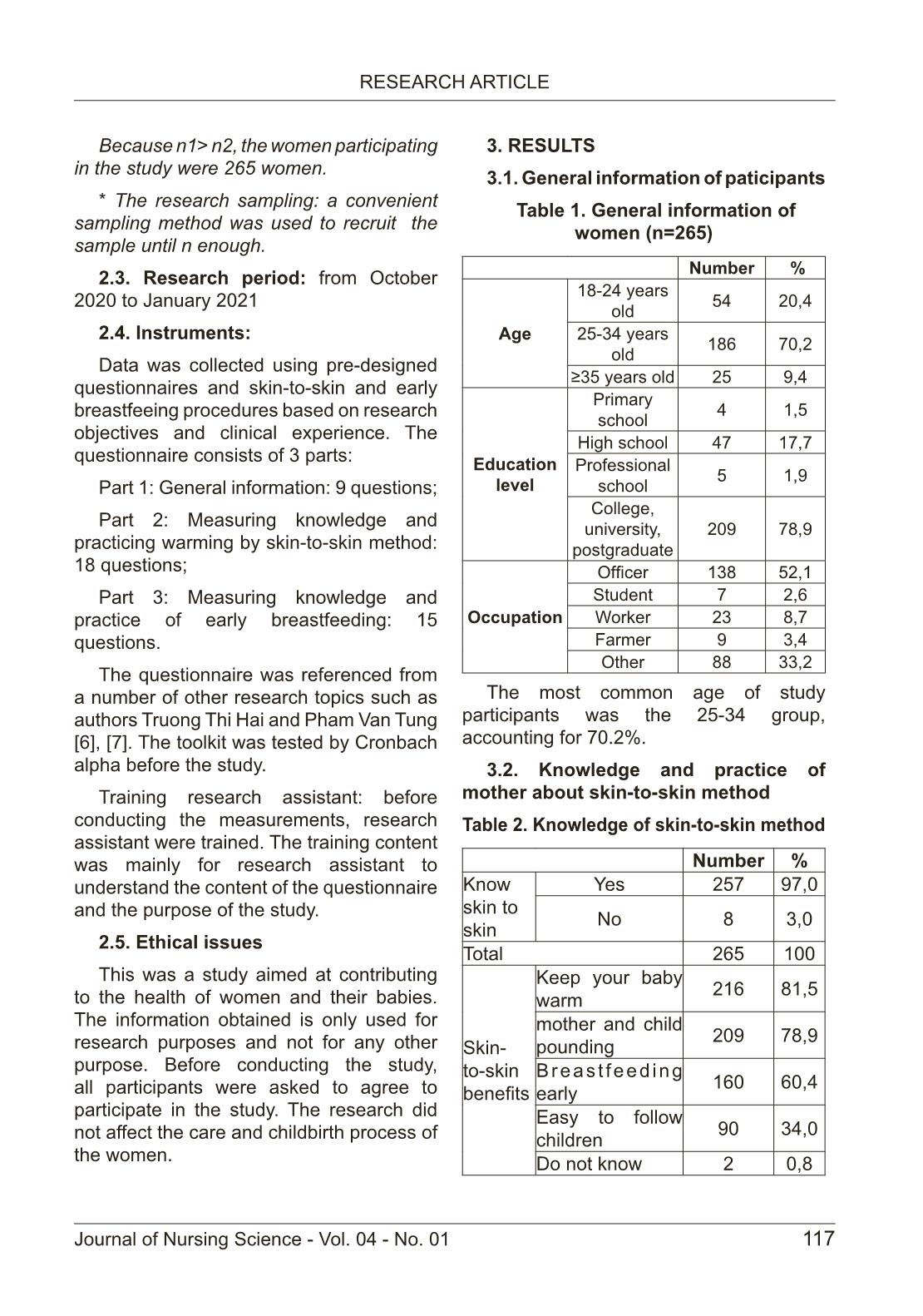
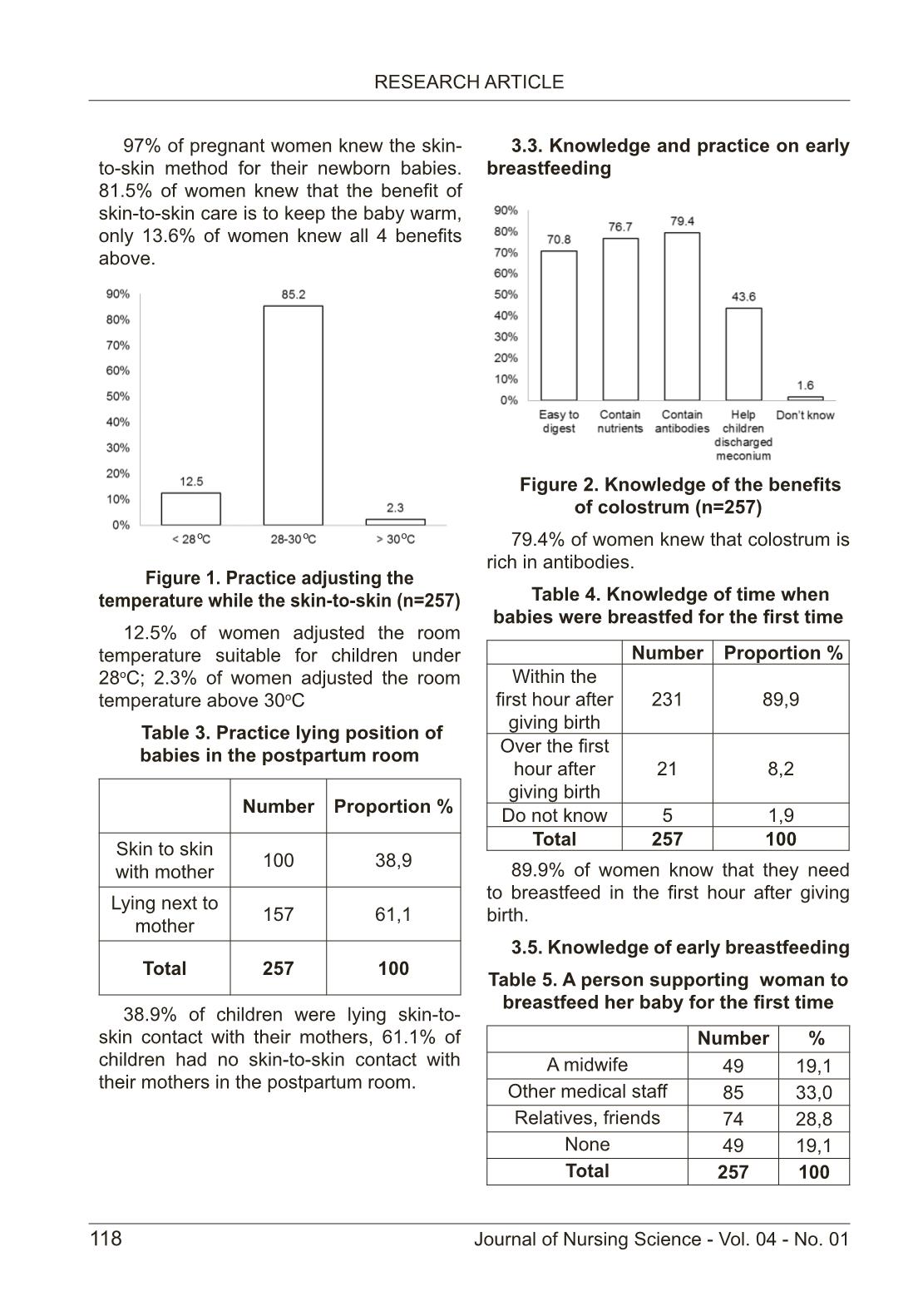
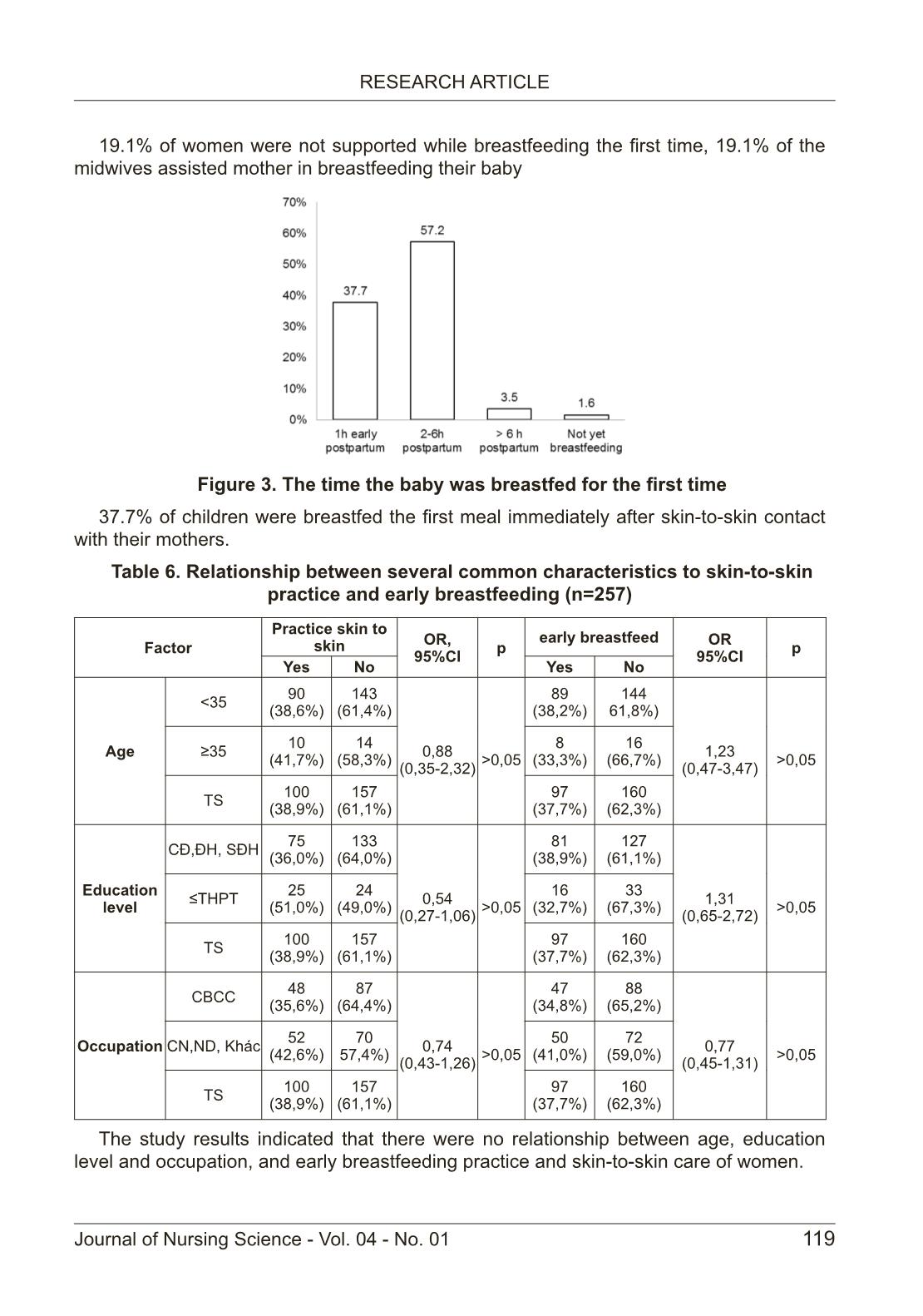
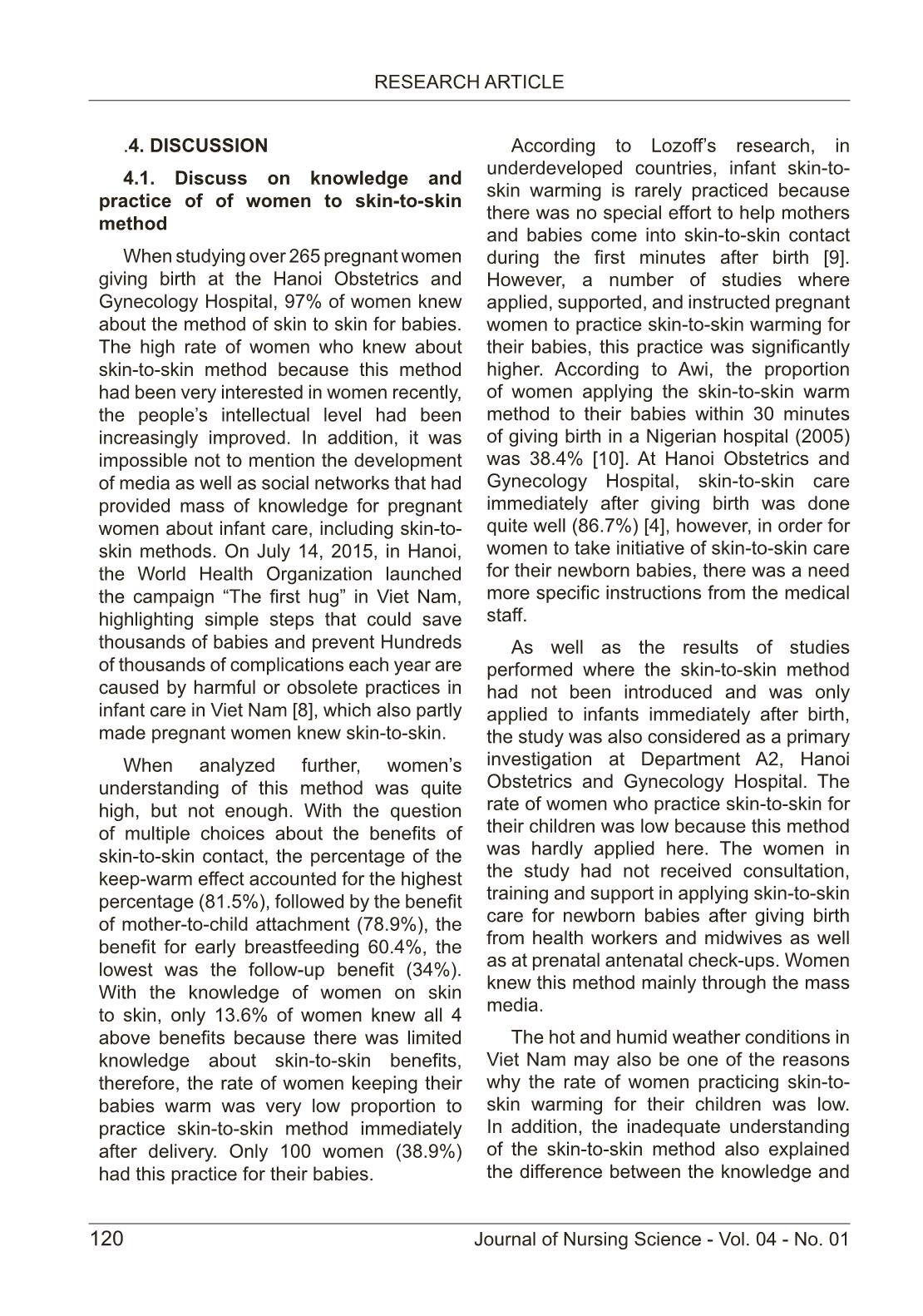
115 RESEARCH ARTICLE Journal of Nursing Science - Vol. 04 - No. 01 KNOWLEDGE AND PRACTICE ON SKIN-TO-SKIN CONTACT AND EARLY BREASTFEEDING METHODS OF WOMEN WITH VAGINAL DELIVERY AT HA NOI OBSTETRICS AND GYNECOLOGY HOSPITAL Pham Thuy Quynh1, Pham Van Tan1, Tran Mai Huyen1, Pham Thi Kim Hoan1, Le Tung Lam1 1Hanoi Medical College ABSTRACT Objective: To describe the knowledge, practice of skin to skin and early breastfeeding of women with vaginal delivery at the Hanoi Obstetrics and Gynecology Hospital. 2. To examine the factors related to the practice of skin-to- skin and early breastfeeding of women with vaginal delivery at the Hanoi Obstetrics and Gynecology Hospital. Method: Postpartum women at ward A2, Hanoi Obstetrics and Gynecology Hospital were recruited to the study. Results: 97% of pregnant women knew the method of skin-to-skin treatment for their infants; 81.5% of the women knew that the benefit of skin-to-skin care is to keep the baby warm; Only 38.9% of infants were allowed to skin-to-skin contact with their mothers in the postpartum room. 79.4% of pregnant women reported that colostrum is rich in antibodies, 37.7% of children were breastfed immediately after skin-to-skin contact with mother; 19.1% of women were not supported while breastfeeding the first meal, 19.1% of the women were assisted to breastfeed their baby. No relationship has been found between women ’s age, education and occupation, and skin-to- skin practice and early breastfeeding. Conclusion: 38.9% of children were skin- to-skin contact with their mothers in the postpartum room; 37.7% of children were breastfed the immediately after skin-to-skin contact with their mothers. Keywords: Knowledge, practice, skin to skin, early breastfeeding 1. INTRODUCTION Newborn health care is a problem that is attracting the attention of countries around the world. Therefore, the Ministry of Health identified infant health as a priority in the National Child Survival Action Plan for the period 2015-2020 [1] According to UNICEF, in Viet Nam, the report on survey of children and women objectives (MICS 2014) found that only 24.3% of children under 6 months of age were exclusively breastfed and only about 26.5 % of infants were breastfed within the first hour of life [2]. EENC implementation in 8 priority countries in the Western Pacific, only 32% of children were breastfed before isolating with mother. The consequences of neonatal morbidity and mortality were severe, and interventions available within the maternity- child health care program may save the lives of most infants. Warm incubation with skin-to-skin method and early breastfeeding were simple and easy interventions that contributed to improving health and reducing infant mortality. In addition to adjusting body temperature, the skin-to- Cor. author: Pham Thuy Quynh Email: phamthuyquynhcdythn@gmail.com Received: Feb 08, 2021 Revised: Feb 15, 2021 Accepted: Mar 05, 2021 116 RESEARCH ARTICLE Journal of Nursing Science - Vol. 04 - No. 01 skin method between mother and infant immediately after birth also had many other effects such as: increasing the rate of early and exclusive breastfeeding, increasing the affection of mother and child, developing cognitition, reducing stress, and reducing infections in infants [1], [3]. Hanoi Obstetrics and Gynecology Hospital always wants to take care of pregnant women and newborns with the new and most effective methods. In order to be able to apply skin-to-skin and early lactation in the first days after birth, there is a need to assess the practice of women on skin- to-skin and early breastfeeding of women after giving birth. Therefore, the research was conducted with 2 objectives: Describe the current state of knowledge, practice of skin to skin and early breastfeeding of women after giving birth at Hanoi Obstetrics and Gynecology Hospital. Examine factors related to skin-to-skin practice and early breastfeeding of women after giving birth at Hanoi Obstetrics and Gynecology Hospital. 2. RESEARCH METHOD 2.1. Participants: Postpartum women at ward A2, Hanoi Obstetrics and Gynecology Hospital were recruited to the study. 2.1.1. Inclusion criteria: - Over 18 years; - Fullterm pregnancy from 37-41 weeks as expected; - Healthy babies; - Can speak, read, listen and understand VietNamese; - Volunteer to participate in research; 2.1.2. Exclusion criteria: - Women with deformity; - Women with some internal and surgical diseases: cardiovascular, hypertension, bronchial asthma, ... - Women with cognitive impairment. 2.2. Methods: 2.2.1. Research design: The research used cross-sectional descriptive design. 2.2.2. Sample size: * Skin to skin part Sample size using the formula for descriptive study: n= z2(1- a/2)p(1-p)/d2 * In which: n: required sample size; a ... skin care of women. 120 RESEARCH ARTICLE Journal of Nursing Science - Vol. 04 - No. 01 .4. DISCUSSION 4.1. Discuss on knowledge and practice of of women to skin-to-skin method When studying over 265 pregnant women giving birth at the Hanoi Obstetrics and Gynecology Hospital, 97% of women knew about the method of skin to skin for babies. The high rate of women who knew about skin-to-skin method because this method had been very interested in women recently, the people’s intellectual level had been increasingly improved. In addition, it was impossible not to mention the development of media as well as social networks that had provided mass of knowledge for pregnant women about infant care, including skin-to- skin methods. On July 14, 2015, in Hanoi, the World Health Organization launched the campaign “The first hug” in Viet Nam, highlighting simple steps that could save thousands of babies and prevent Hundreds of thousands of complications each year are caused by harmful or obsolete practices in infant care in Viet Nam [8], which also partly made pregnant women knew skin-to-skin. When analyzed further, women’s understanding of this method was quite high, but not enough. With the question of multiple choices about the benefits of skin-to-skin contact, the percentage of the keep-warm effect accounted for the highest percentage (81.5%), followed by the benefit of mother-to-child attachment (78.9%), the benefit for early breastfeeding 60.4%, the lowest was the follow-up benefit (34%). With the knowledge of women on skin to skin, only 13.6% of women knew all 4 above benefits because there was limited knowledge about skin-to-skin benefits, therefore, the rate of women keeping their babies warm was very low proportion to practice skin-to-skin method immediately after delivery. Only 100 women (38.9%) had this practice for their babies. According to Lozoff’s research, in underdeveloped countries, infant skin-to- skin warming is rarely practiced because there was no special effort to help mothers and babies come into skin-to-skin contact during the first minutes after birth [9]. However, a number of studies where applied, supported, and instructed pregnant women to practice skin-to-skin warming for their babies, this practice was significantly higher. According to Awi, the proportion of women applying the skin-to-skin warm method to their babies within 30 minutes of giving birth in a Nigerian hospital (2005) was 38.4% [10]. At Hanoi Obstetrics and Gynecology Hospital, skin-to-skin care immediately after giving birth was done quite well (86.7%) [4], however, in order for women to take initiative of skin-to-skin care for their newborn babies, there was a need more specific instructions from the medical staff. As well as the results of studies performed where the skin-to-skin method had not been introduced and was only applied to infants immediately after birth, the study was also considered as a primary investigation at Department A2, Hanoi Obstetrics and Gynecology Hospital. The rate of women who practice skin-to-skin for their children was low because this method was hardly applied here. The women in the study had not received consultation, training and support in applying skin-to-skin care for newborn babies after giving birth from health workers and midwives as well as at prenatal antenatal check-ups. Women knew this method mainly through the mass media. The hot and humid weather conditions in Viet Nam may also be one of the reasons why the rate of women practicing skin-to- skin warming for their children was low. In addition, the inadequate understanding of the skin-to-skin method also explained the difference between the knowledge and 121 RESEARCH ARTICLE Journal of Nursing Science - Vol. 04 - No. 01 practice levels of women (81.5% of women knew but only 38.9% practiced to warm the baby). To prevent hypothermia in infants, the ideal room temperature should be 28-30ºc. In this study, it was also shown that 12.5% of women said that the room temperature should only be below 28oC, which also greatly affected the hypothermia of the newborn. Especially in the total number of newborns dying at the hospital in the first 24 hours after delivery, up to 32% of mothers showed signs of hypothermia. A study in Hai Phong showed that hypothermia accounted for 35% of all neonatal deaths [11]. The results in the study showed that it was necessary to further improve the understanding of pregnant women and health workers about knowledge and practice of keeping warm babies after birth, through communication, education. Providing appropriate information may limit hypothermia, prevent morbidity and mortality related to the cause of hypothermia in infants. 4.2. Discuss on knowledge and practice about early breastfeeding for women Breast milk is the best food for babies and young children. Women ‘s knowledge about the benefits of colostrum was relatively high. Up to 79.4% of women knew that colostrum contained many antibodies and 76.7% knew colostrum contained many nutrients. Meanwhile, according to research results of Le Thi Yen Phi, the number of women who knew the benefits of colostrum was 95% and that of Truong Thi Hai was 99.8% [6], [12]. Along with the proportion of women who knew the concept of colostrum, the women who had the correct knowledge about the time of first breastfeeding in the study accounted for 89.9% of them that they should breastfeed immediately after birth. This proved that the knowledge of breastfeeding timing after giving birth of women was very good, it was quite reasonable because 76.7% of women believed that colostrum contained many antibodies, helping the baby increase resistance. The results were higher than those of Ton Thi Anh Tu and Nguyen Thu Tinh while the number of women who believed that breastfeeding within the first hour after birth was 69.45% [13]. Although the knowledge of breastfeeding timing and the benefits of early breastfeeding was quite good, the results showed that the proportion of women who breastfeed within the first hour after birth was quite low. (37.7%), most children (57.2%) were breastfed after the first 2-6 hours postpartum. Currently, breastfeeding was a popular practice in the world, however, the rate of breastfeeding within the first hour after birth was generally low. In Asia, only nearly 20% of babies were breastfed within the first 24 hours of life. Research in Jinan City, China showed that 51% of women breastfed for the first time after an hour According to a study by Le Thi Huong and Do Huu Hanh in Yen Bai province in 2008, 66% of pregnant women breastfed early within the first half hour after birth [14]. The reasons not to breastfeed within the first hour of birth were mainly due to lack of understanding of the benefits of colostrum, the benefits of early breastfeeding, and in many places, old and long-term customs of local life or tired women after birth. Only 19.1% of the women received the assistance of the midwife to breastfeed their baby and 33% were from other health workers. Department of Pediatrics A2 is assigning care to teams, groups, so each team and group will have their own specific work, such as taking care of pregnant women in labor, taking care of women after giving birth. Care for pregnant women in stage II labor also needed to better complete counseling 122 RESEARCH ARTICLE Journal of Nursing Science - Vol. 04 - No. 01 and support for the baby to breastfeed the first breast-feeding meal. For that reason, 19.1% of women were not supported to breastfeed their babies, so they ate some other foods to replace breast milk. This was completely not beneficial for the newborn because the baby does not receive breast milk with antibodies. In India, 70% of the rural women and more than 50% of the educated women in Bombay gave their babies other foods and drinks before the first breastfeeding. Another study by Chhabra in Delhi, India also showed that 76.9% of babies were given other foods and drinks before their first breast-feeding. In some rural Nigeria, 100% of women gave their babies water, formula or herbal tea before their first breastfeed [15]. The results above showed that this practice was very popular in many countries. In Asia, usually babies were not fed colostrum and so the first feeding usually occurs after 24 hours after birth. According to the population and health survey, only 28% of newborns were breastfed for one hour after giving birth, while other babies were fed cow’s milk, honey before the first breastfeeding. The high rate of women giving another food / drink before the first breastfeeding (19.1%) reflected the situation of infants not exclusively breastfed in the first 6 months. 4.3. Discussion on factors related to practice of skin-to-skin and early breastfeeding of women The results of the study were not similar to that of Truong Thi Hai, in this result, skin- to-skin practice in mothers of the group above 35 and group below 35 had no difference, no statistical significance with p> 0.05. In Truong Thi Hai’s study, maternal education was related to skin-to-skin warming practice. Specifically, in those with higher educational attainment (intermediate and above), the practice rate of skin-to-skin warming was 11.9 times higher with OR = 11.9; 95% CI (1.9 - 489.7) [6]. Another study conducted in Nigerian mothers in 2004 on skin-to-skin contact practice found that maternal education did not have a statistically significant effect on skin-to-skin practice. The research results showed that mother’s education level was similar to the above results on skin-to-skin practice and early postpartum breastfeeding. Specifically, for mothers’ education, those with college, university or post-graduate education had practiced breastfeeding within the first hour after birth (38.9%) for women with upper secondary education (32.7%), however this difference was statistically significant with p <0.05. Other maternal factors, such as occupation, did not have a statistically significant effect on the first breastfeeding within one hour of birth. Maternal education was considered to be the most important factor in deciding to practice breastfeeding. The knowledge and skills to find information to help mothers grasp information about the benefits of colostrum for babies as well as the benefit of breastfeeding the infant early on to herself shortly after birth, however, within this study no association between education level and skin-to-skin practice and early breastfeeding was found. However, the research results on this relationship were also very different, this relationship must also take into account the interaction between factors of individual characteristics with the living environment, and access to health care services. 5. CONCLUSION - 97% of women knew the method of skin-to-skin for their newborns, 81.5% of women knew that the benefit of skin-to-skin care was keeping their babies warm, and only 38.9% of babies had skin-to-skin-to- skin care in the postpartum room. - 79.4% of women knew that colostrum was rich in antibodies, 37.7% of children were breastfed for the first time after skin- 123 RESEARCH ARTICLE Journal of Nursing Science - Vol. 04 - No. 01 to-skin contact with mothers; - There was no relationship between the age, education level and occupation and the skin-to-skin practice and early breastfeeding of women. REFERENCES 1. Ministry of Health (2016). National action plan on maternal, infant and child health care for the period 2016 - 2020, issued together with Decision 4177 / QD- BYT, dated August 3, 2016. [In VietNamese] 2. UNICEF (2014). The 2013-2014 Mother and Infant Goals and Goals Assessment Survey, General Statistics Office Publisher, Hanoi. [In VietNamese] 3. Charpak N., Ruiz J.G., Zupan J. et al, (2005). Kangaroo Mother Care: 25 years after. Acta Paediatr Oslo Nor 1992, (94), 514–522 4. Pham Thuy Quynh (2018). Assessment of maternal satisfaction and the situation of essential care for mothers and infants during and immediately after birth at Hanoi Obstetrics and Gynecology Hospital in 2018, Master Thesis of Nursing, Nam Dinh University of Nursing. [In VietNamese] 5. Le Thi Mong Tuyen and Tran Dinh Le Khanh (2016). Evaluate the results of applying essential care procedures for mothers and newborns during and immediately after delivery at the Da Nang Obstetrics and Pediatrics Hospital Department. Da Nang Obstetrics & Pediatrics Hospital, December 2016. [In VietNamese] 6. Truong Thi Hai (2016). Knowledge and practice on skin-to-skin warming and early breastfeeding methods of women at Bach Mai Hospital. Bachelor of Arts in Nursing, Hanoi Medical University. [In VietNamese] 7. Pham Van Tung (2017). Changes in awareness of breastfeeding among mothers with children aged 0-6 months in Nam Dinh city in 2017 after educational intervention, Master’s thesis in nursing, Nam Dinh University of Nursing. [In VietNamese] 8. Western Pacific Regional Office (2015). Infant Health. who.int/Viet Nam/topics /newborn_health/ factsheet/en/ 9. Lozoff B. (1983). Birth and ‘bonding’ in non-industrial societies. Dev Med Child Neurol, (25), 595–600. 10. Awi D.D. & Alikor E. a. D. (2004). The influence of pre- and post-partum factors on the time of contact between mother and her new-born after vaginal delivery. Niger J Med J Natl Assoc Resid Dr Niger, (13), 272–275. 11. Doan Thi Thanh Huong (1998). Relationship between weight, temperature and Apgar score at birth and neonatal mortality. Hai Phong 1996-1997. The fourth scientific conference of Hanoi Medical University. [In VietNamese] 12. Le Thi Yen Phi (2009). Knowledge, attitudes and practices of breastfeeding for postpartum mothers at Hung Vuong Hospital in 2009. Hung Vuong Hospital. [In VietNamese] 13. Ton Thi Anh Tu and Nguyen Thu Tinh (2011). Knowledge, attitudes and practices on breastfeeding of mothers with children under six months old at Children’s Hospital I from December 1, 2009 to April 30, 2010. [In VietNamese] 14. Le Thi Huong and Do Huu Hanh (2008). Maternal knowledge of nutritional practices and children’s nutritional status in Yen Bai province. [In VietNamese] 15. Prasad B. & Costello A.M. (1995). Impact and sustainability of a “baby friendly” health education intervention at a district hospital in Bihar, India. BMJ, (310), 621–623.
File đính kèm:
 knowledge_and_practice_on_skin_to_skin_contact_and_early_bre.pdf
knowledge_and_practice_on_skin_to_skin_contact_and_early_bre.pdf

