High dose chemotherapy and autologous hematopoietic stem cell rescue for children with high risk neuroblastoma: Two case report
Introduction: High-risk neuroblastoma is a childhood malignancy with a poor prognosis. Gradual
improvements in survival have correlated with therapeutic intensity, and the ability to harvest, process and
store autologous hematopoietic stem cells has allowed for dose intensification beyond marrow tolerance.
Case: We report two cases which were diagnosed high risk neuroblastoma. The first case had big
heterogeneous at his left adrenal gland with metastasis in bone marrow and his brain. The second case
with localised tumor at her right kidney and NMYC positive. Both cases were treated with SIOPEN protocol,
starting with 8 course RAPID COJECT. Patients had partial response and were collected stem cells. Then
they were primary tumor resection; receiving high dose chemotherapy with autologous- stem cell rescue,
radiation and retino acid treatment, respectively.
Conclusion: This is initially report of autologous stem cell transpant for high risk neuroblastoma. Even
only two patients, the results showed that stem cell transplant was safe and effective. We are continuing
to implement for more case with high risk neuroblastoma and will have better report with a bigger number.

Trang 1
Trang 2
Trang 3

Trang 4
Trang 5
Tóm tắt nội dung tài liệu: High dose chemotherapy and autologous hematopoietic stem cell rescue for children with high risk neuroblastoma: Two case report

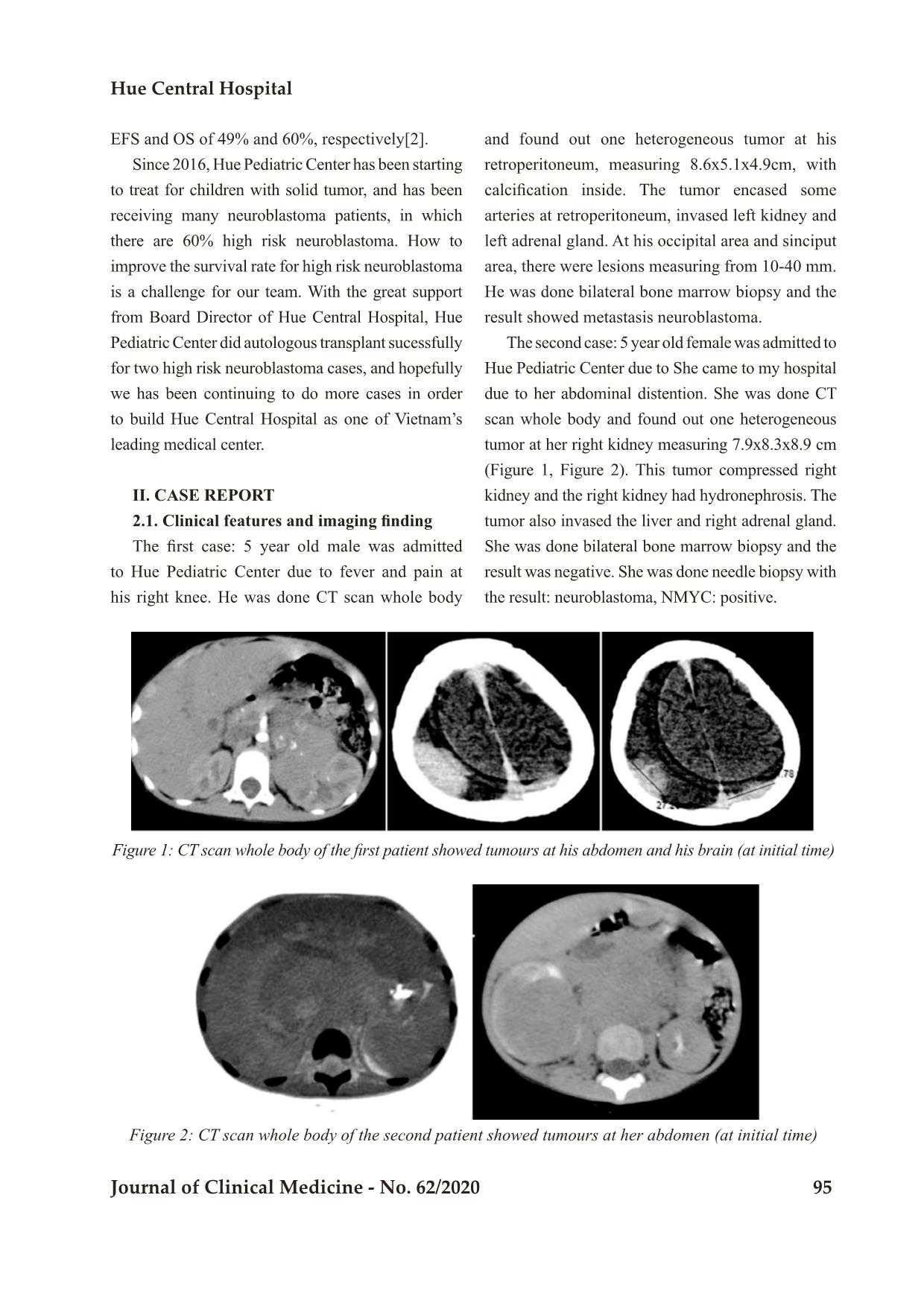
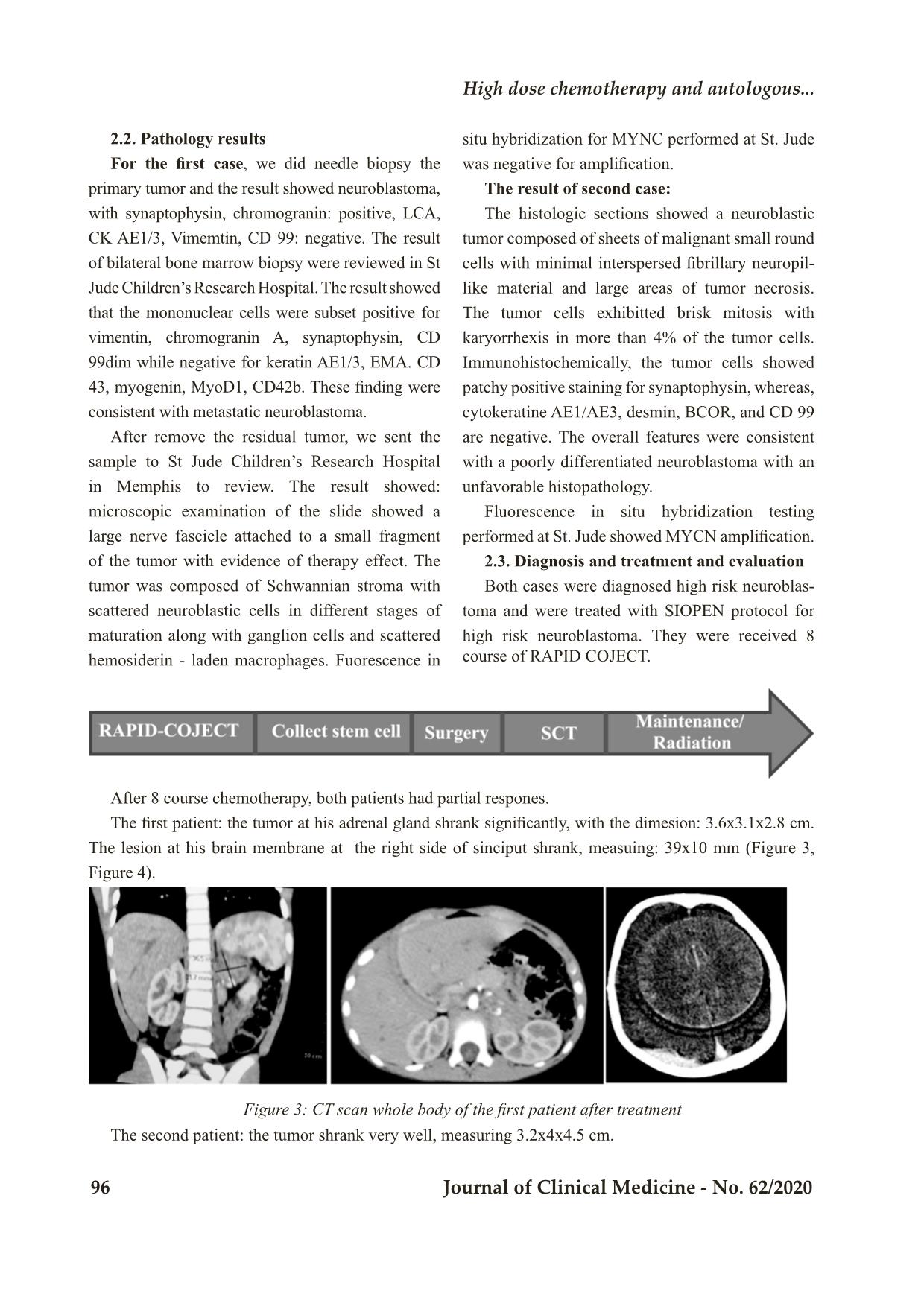
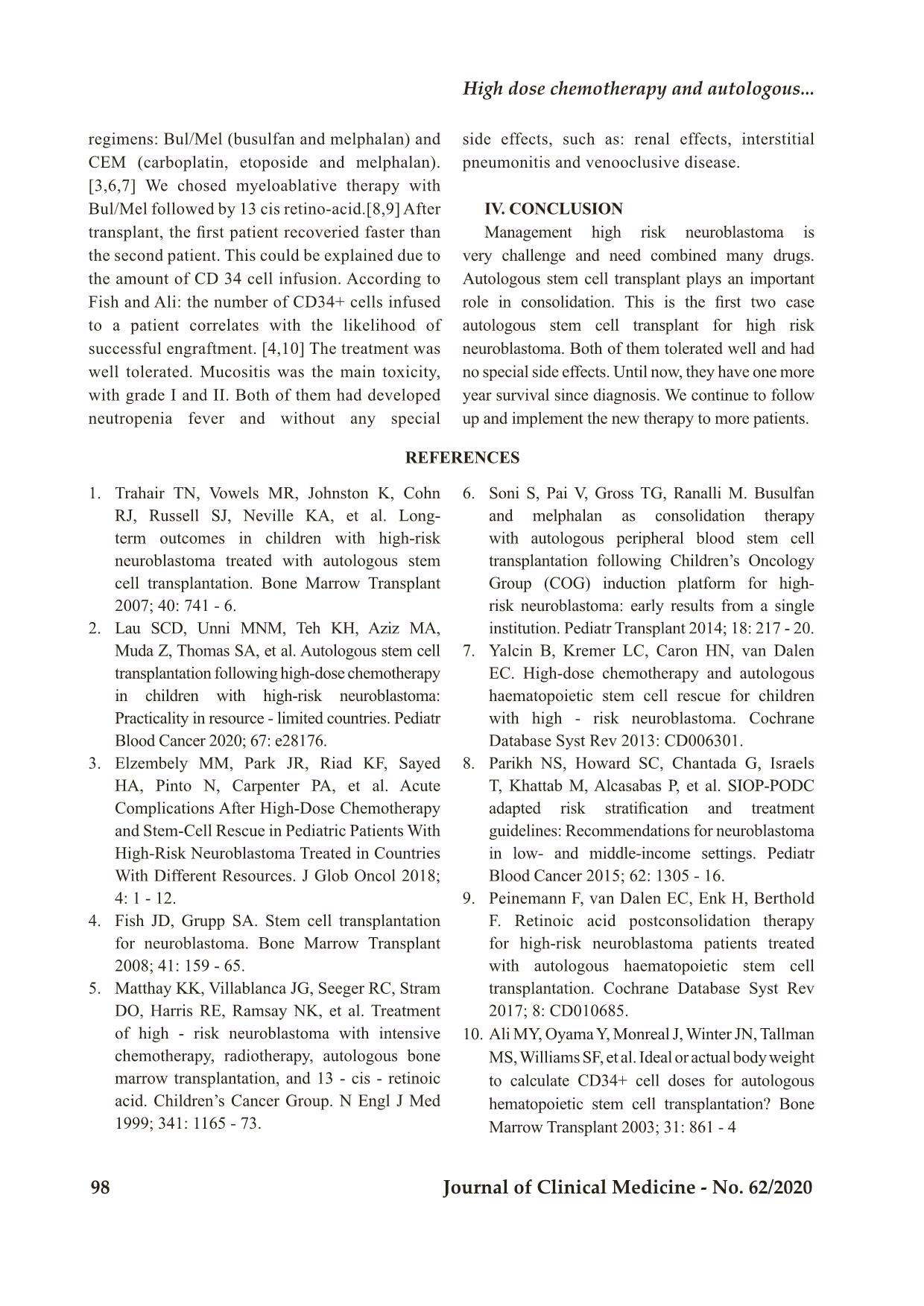
Bệnh viện Trung ương Huế 94 Journal of Clinical Medicine - No. 62/2020 HIGH DOSE CHEMOTHERAPY AND AUTOLOGOUS HEMATOPOIETIC STEM CELL RESCUE FOR CHILDREN WITH HIGH RISK NEUROBLASTOMA: TWO CASE REPORT Nguyen Thi Kim Hoa1, Tran Kiem Hao1, Chau Van Ha1, Phan Canh Duy2, Dong Si Sang3, Phan Thi Thuy Hoa3, Ho Huu Thien4, Nguyen Thi My Linh1, Pham Nhu Hiep4 DOI: 10.38103/jcmhch.2020.62.16 ABSTRACT Introduction: High-risk neuroblastoma is a childhood malignancy with a poor prognosis. Gradual improvements in survival have correlated with therapeutic intensity, and the ability to harvest, process and store autologous hematopoietic stem cells has allowed for dose intensification beyond marrow tolerance. Case: We report two cases which were diagnosed high risk neuroblastoma. The first case had big heterogeneous at his left adrenal gland with metastasis in bone marrow and his brain. The second case with localised tumor at her right kidney and NMYC positive. Both cases were treated with SIOPEN protocol, starting with 8 course RAPID COJECT. Patients had partial response and were collected stem cells. Then they were primary tumor resection; receiving high dose chemotherapy with autologous- stem cell rescue, radiation and retino acid treatment, respectively. Conclusion: This is initially report of autologous stem cell transpant for high risk neuroblastoma. Even only two patients, the results showed that stem cell transplant was safe and effective. We are continuing to implement for more case with high risk neuroblastoma and will have better report with a bigger number. 1. Pediatric Center, Hue Central Hospital 2. Oncology Center, Hue Central Hospital 3. Blood and Transfusion Center, Hue Central Hospital 4. Department of Abdominal Emergency and Pediatric Surgery, Hue Central Hospital Corresponding author: Nguyen Thi Kim Hoa Email: kimhoa.fmi@gmail.com Received: 8/5/2020; Revised: 17/5/2020 Accepted: 20/6/2020 I. INTRODUCTION Neuroblastoma is the most common extracranial solid tumor in children[1], accounting for 7% to 8% of all childhood cancers. The prevalence is about 1 case per 7.000 live births. Neuroblastoma is slightly more common in boys than in girls, with a male to female ratio of 1.1 to 1. The peak incidence occurs at 2 years of age, some studies show that 89% are younger than 5 years, and 98% of cases are diagnosed in the first 10 years of life. The distribution of cases by age clearly shows that this is a disease of infancy and early childhood, with the highest number of cases diagnosed in the first month of life. Before the development of comprehensive, multimodality therapy, long term survival probabilities for high risk neuroblastoma patient were less than 15% [2]. High dose chemotherpay with autologous stem cell rescue has improved the outcomes for children with high risk neuroblastoma [3,4]. Using busulfan and melphalan (BuMel) as conditioning regime, the International Society of Pediatric Oncology Neuroblastoma HR NBL1 protocol reported 3 year High dose chemotherapy and autologous... Hue Central Hospital Journal of Clinical Medicine - No. 62/2020 95 EFS and OS of 49% and 60%, respectively[2]. Since 2016, Hue Pediatric Center has been starting to treat for children with solid tumor, and has been receiving many neuroblastoma patients, in which there are 60% high risk neuroblastoma. How to improve the survival rate for high risk neuroblastoma is a challenge for our team. With the great support from Board Director of Hue Central Hospital, Hue Pediatric Center did autologous transplant sucessfully for two high risk neuroblastoma cases, and hopefully we has been continuing to do more cases in order to build Hue Central Hospital as one of Vietnam’s leading medical center. II. CASE REPORT 2.1. Clinical features and imaging finding The first case: 5 year old male was admitted to Hue Pediatric Center due to fever and pain at his right knee. He was done CT scan whole body and found out one heterogeneous tumor at his retroperitoneum, measuring 8.6x5.1x4.9cm, with calcification inside. The tumor encased some arteries at retroperitoneum, invased left kidney and left adrenal gland. At his occipital area and sinciput area, there were lesions measuring from 10-40 mm. He was done bilateral bone marrow biopsy and the result showed metastasis neuroblastoma. The second case: 5 year old female was admitted to Hue Pediatric Center due to She came to my hospital due to her abdominal distention. She was done CT scan whole body and found out one heterogeneous tumor at her right kidney measuring 7.9x8.3x8.9 cm (Figure 1, Figure 2). This tumor compressed right kidney and the right kidney had hydronephrosis. The tumor also invased the liver and right adrenal gland. She was done bilateral bone marrow biopsy and the result was negative. She was done needle biopsy with the result: neuroblastoma, NMYC: positive. Figure 1: CT scan whole body of the first patient showed tumours at his abdomen and his brain (at initial time) Figure 2: CT scan whole body of the second patient showed tumours at her abdomen (at initial time) Bệnh viện Trung ương Huế 96 Journal of Clinical Medicine - No. 62/2020 2.2. Pathology results For the first case, we did needle biopsy the primary tumor and the result showed neuroblastoma, with synaptophysin, chromogranin: positive, LCA, CK AE1/3, Vimemtin, CD 99: negative. The result of bilateral bone marrow biopsy were reviewed in St Jude Children’s Research Hospital. The result showed that the mononuclear cells were subset positive for vimentin, chromogranin A, synaptophysin, CD 99dim while negative for keratin AE1/3, EMA. CD 43, myogenin, MyoD1, CD42b. These finding were consistent with metastatic neuroblastoma. After remove the residual tumor, we sent the sample to St Jude Children’s Research Hospital in Memphis to review. The result showed: microscopic examination of the slide showed a large nerve fascicle attached to a small fragment of the tumor with evidence of therapy effect. The tumor was composed of Schwannian stroma with scattered neuroblastic cells in different stages of maturation along with ganglion cells and scattered hemosiderin - laden macrophages. Fuorescence in situ hybridization for MYNC performed at St. Jude was negative for amplification. The result of second case: The histologic sections showed a neuroblastic tumor composed of sheets of malignant small round cells with minimal interspersed fibrillary neuropil- like material and large areas of tumor necrosis. The tumor cells exhibitted brisk mitosis with karyorrhexis in more than 4% of the tumor cells. Immunohistochemically, the tumor cells showed patchy positive staining for synaptophysin, whereas, cytokeratine AE1/AE3, desmin, BCOR, and CD 99 are negative. The overall features were consistent with a poorly differentiated neuroblastoma with an unfavorable histopathology. Fluorescence in situ hybridization testing performed at St. Jude showed MYCN amplification. 2.3. Diagnosis and treatment and evaluation Both cases were diagnosed high risk neuroblas- toma and were treated with SIOPEN protocol for high risk neuroblastoma. They were received 8 course of RAPID COJECT. After 8 course chemotherapy, both patients had partial respones. The first patient: the tumor at his adrenal gland shrank significantly, with the dimesion: 3.6x3.1x2.8 cm. The lesion at his brain membrane at the right side of sinciput shrank, measuing: 39x10 mm (Figure 3, Figure 4). Figure 3: CT scan whole body of the first patient after treatment The second patient: the tumor shrank very well, measuring 3.2x4x4.5 cm. High dose chemotherapy and autologous... Hue Central Hospital Journal of Clinical Medicine - No. 62/2020 97 Figure 4: CT scan whole body of the second patient after treatment With the partial reponses, both patients were collected stem cells. The first patient had 4.11x 106 CD 34 cells, the second patient had 2.87x106 CD 34 cells. Then, both of them was removed than 80% original tumors, and were ready for stem cell transplantation. 2.4. High dose chemotherapy and stem cell transplantation Both patients were received conditioning regimen with Bul/Mel as the below: Medicine - 7 - 6 -5 -4 -3 -2 -1 0 Busulfan IV xx xxxx xxxx xxxx xx Melphalan IV x Hydration 3l/m2/d x x x x x x x Stem cell infusion x Mephalan dose: 140mg/m2/day, Busulfan dose: 1mg/kg/day. During transplant, patient were received ursodiol 300mg/m2/day (from D-8 to D+80 to prevent VOD; Acyclovir 250mg/m2 every 8 hours from D-8 đến D 100. Levofloxacine 10mg/kg x 2 times per day (D-8 to D30; G-CSF since D+5 until Neutrophile > 0.5x109/l for two consecutive days, and radiation blood products. After transplant, both patients appeared neutropenic fever, mucosa ulcer with grade I, II, elevated CRP and PCT, and were treated with antibiotic and antifungal. The second case lasted fever for 6 days due to Chromobacterium violaceum infection. The first patient had neutrophile and platelet recovery on day 11 and day 25 respectively. The second patient had neutrophile and platelet recovery on day 42 and day 45 respectively. Both patients were discharged on day 32 and day 72 respectively without any special side effects (kidney, interstitial pneumonitis and venoocclusive diseas). Then they were received radiation to primary tumor, and took 13 cis retino acid. Now, both of them are very healthy: the first patient has completed remission after 13 months, and the second patient has completed remission after 12 months.. III. DISCUSSION The diagnosis of high risk neuroblastoma for both patients were clearly and based on their responses, they had indication to receive high dose chemotherapy and autologous stem cell transplantation.[5] However, due to receiving many chemotherapy, their marrows were often hypocellulary, so the amount of stem cell collection were not high, only 4.11x 106 CD 34 cells for the first case, and 2.87x106 CD 34 cells for the second case. This is a reason why nowadays, they prefer to collect stem cells earlier if patients do not have bone marrow metastasis or bone marrow clears after chemotherpy. [4,6] Regarding conditioning regimen, there are two Bệnh viện Trung ương Huế 98 Journal of Clinical Medicine - No. 62/2020 regimens: Bul/Mel (busulfan and melphalan) and CEM (carboplatin, etoposide and melphalan). [3,6,7] We chosed myeloablative therapy with Bul/Mel followed by 13 cis retino-acid.[8,9] After transplant, the first patient recoveried faster than the second patient. This could be explained due to the amount of CD 34 cell infusion. According to Fish and Ali: the number of CD34+ cells infused to a patient correlates with the likelihood of successful engraftment. [4,10] The treatment was well tolerated. Mucositis was the main toxicity, with grade I and II. Both of them had developed neutropenia fever and without any special side effects, such as: renal effects, interstitial pneumonitis and venooclusive disease. IV. CONCLUSION Management high risk neuroblastoma is very challenge and need combined many drugs. Autologous stem cell transplant plays an important role in consolidation. This is the first two case autologous stem cell transplant for high risk neuroblastoma. Both of them tolerated well and had no special side effects. Until now, they have one more year survival since diagnosis. We continue to follow up and implement the new therapy to more patients. REFERENCES 1. Trahair TN, Vowels MR, Johnston K, Cohn RJ, Russell SJ, Neville KA, et al. Long- term outcomes in children with high-risk neuroblastoma treated with autologous stem cell transplantation. Bone Marrow Transplant 2007; 40: 741 - 6. 2. Lau SCD, Unni MNM, Teh KH, Aziz MA, Muda Z, Thomas SA, et al. Autologous stem cell transplantation following high-dose chemotherapy in children with high-risk neuroblastoma: Practicality in resource - limited countries. Pediatr Blood Cancer 2020; 67: e28176. 3. Elzembely MM, Park JR, Riad KF, Sayed HA, Pinto N, Carpenter PA, et al. Acute Complications After High-Dose Chemotherapy and Stem-Cell Rescue in Pediatric Patients With High-Risk Neuroblastoma Treated in Countries With Different Resources. J Glob Oncol 2018; 4: 1 - 12. 4. Fish JD, Grupp SA. Stem cell transplantation for neuroblastoma. Bone Marrow Transplant 2008; 41: 159 - 65. 5. Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, et al. Treatment of high - risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13 - cis - retinoic acid. Children’s Cancer Group. N Engl J Med 1999; 341: 1165 - 73. 6. Soni S, Pai V, Gross TG, Ranalli M. Busulfan and melphalan as consolidation therapy with autologous peripheral blood stem cell transplantation following Children’s Oncology Group (COG) induction platform for high- risk neuroblastoma: early results from a single institution. Pediatr Transplant 2014; 18: 217 - 20. 7. Yalcin B, Kremer LC, Caron HN, van Dalen EC. High-dose chemotherapy and autologous haematopoietic stem cell rescue for children with high - risk neuroblastoma. Cochrane Database Syst Rev 2013: CD006301. 8. Parikh NS, Howard SC, Chantada G, Israels T, Khattab M, Alcasabas P, et al. SIOP-PODC adapted risk stratification and treatment guidelines: Recommendations for neuroblastoma in low- and middle-income settings. Pediatr Blood Cancer 2015; 62: 1305 - 16. 9. Peinemann F, van Dalen EC, Enk H, Berthold F. Retinoic acid postconsolidation therapy for high-risk neuroblastoma patients treated with autologous haematopoietic stem cell transplantation. Cochrane Database Syst Rev 2017; 8: CD010685. 10. Ali MY, Oyama Y, Monreal J, Winter JN, Tallman MS, Williams SF, et al. Ideal or actual body weight to calculate CD34+ cell doses for autologous hematopoietic stem cell transplantation? Bone Marrow Transplant 2003; 31: 861 - 4 High dose chemotherapy and autologous...
File đính kèm:
 high_dose_chemotherapy_and_autologous_hematopoietic_stem_cel.pdf
high_dose_chemotherapy_and_autologous_hematopoietic_stem_cel.pdf

