Dentifying the etiological profile of children presented with hepatomegaly admitted to a tertiary care hospital
Objectives: To identify the pattern and etiology of diseases in children presented hepatomegaly at
Pediatrics Department in Hue Central Hospital, Vietnam.
Material and Methods: The Present study was conducted to evaluate the possible etiology and clinical
features of children presented with hepatomegaly. A total of 107 children, from one month to fifteen years
of age with hepatomegaly admitted in the Pediatric Department of Hue Central Hospital, Vietnam from May
2018 to April 2019 were included in this study.
Results:The most common causes of hepatomegaly were inflammation/infection of the liver (miscellaneous
cause included), hematological diseases and congestion heart failure with the percentage of 50.5%; 27,1%
and 12,1%; respectively. Among the hepatitis group, viral agents account for nearly 50.0%, of which the
most common one was Cytomegalovirus accounting for nearly 30.0%. Distribution of causes by age group
revealed most cases in 1 year-old or younger children was caused by inflammation (53.8%), and in the older
than 1 year-old children were hematological disorders (47.3%) which has statistical significance (P<0.05).
Conclusions: Our research observed that the most common causes of the group of ≤ 1 year old were
hepatitis, followed by cardiovascular disease and biliary obstruction due to congenital biliary atresia, and in
the older than 1 year group, hematological disorders was the most common.
Trang 1
Trang 2
Trang 3
Trang 4
Trang 5
Trang 6
Trang 7
Trang 8
Trang 9
Tóm tắt nội dung tài liệu: Dentifying the etiological profile of children presented with hepatomegaly admitted to a tertiary care hospital
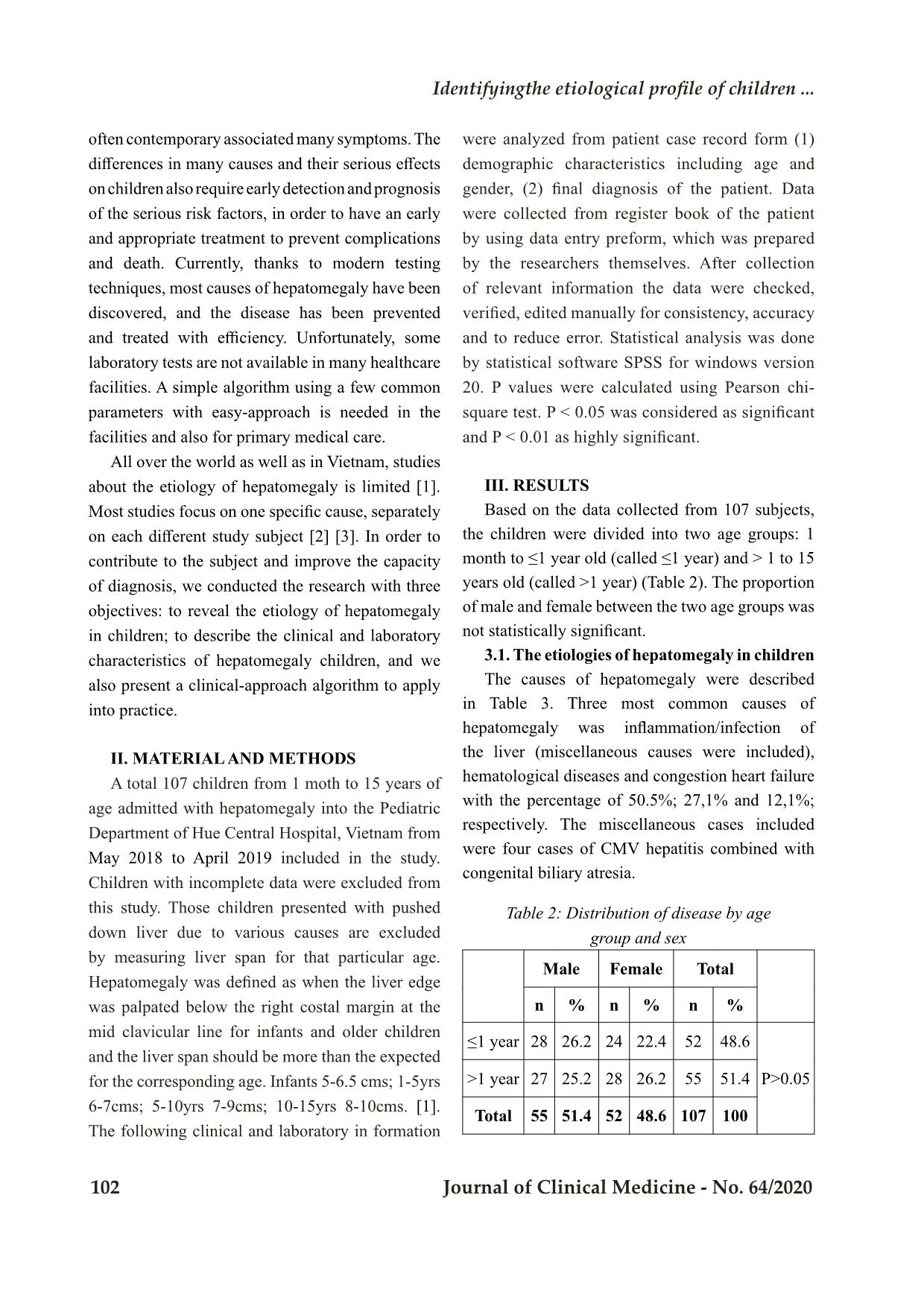
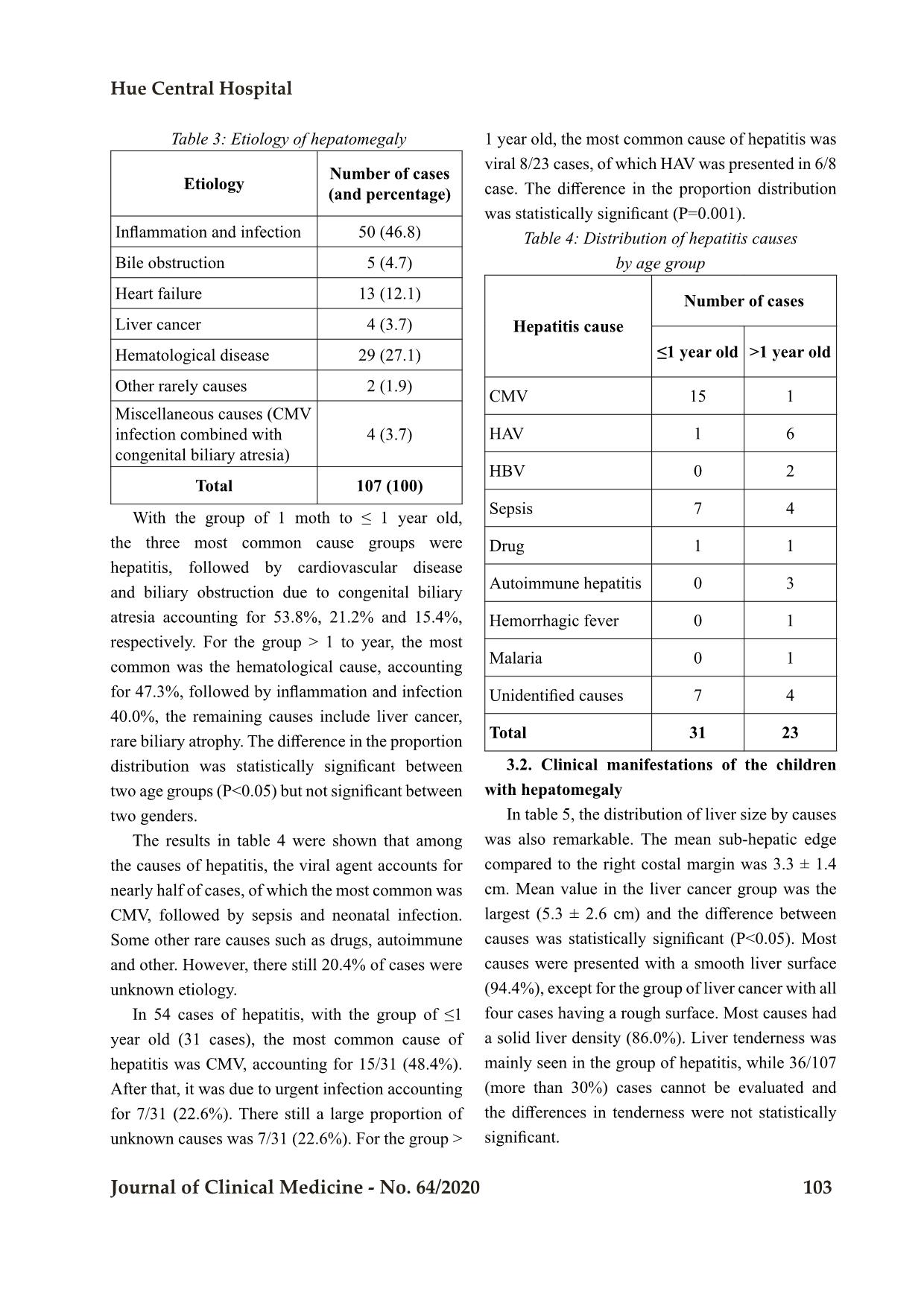
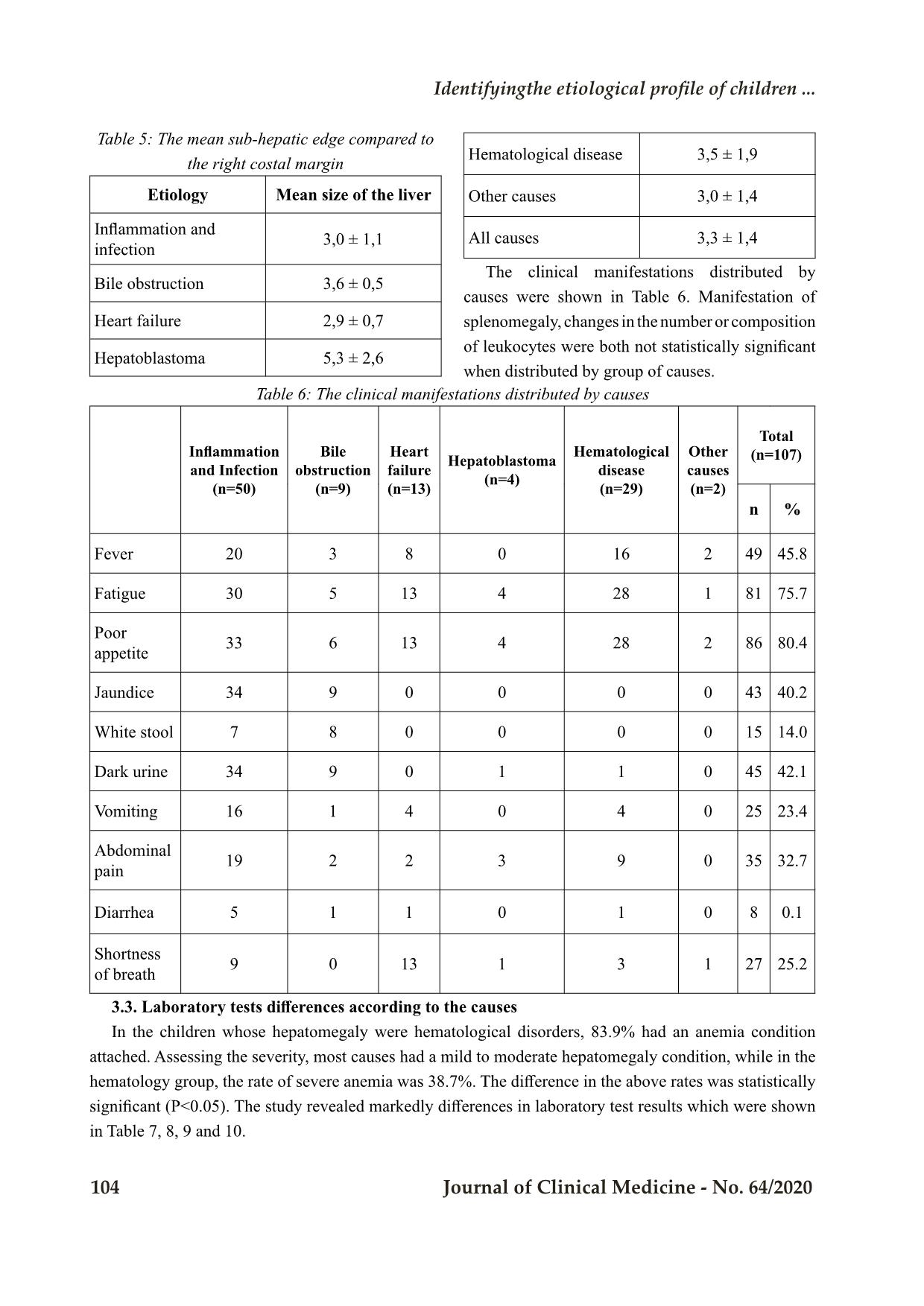
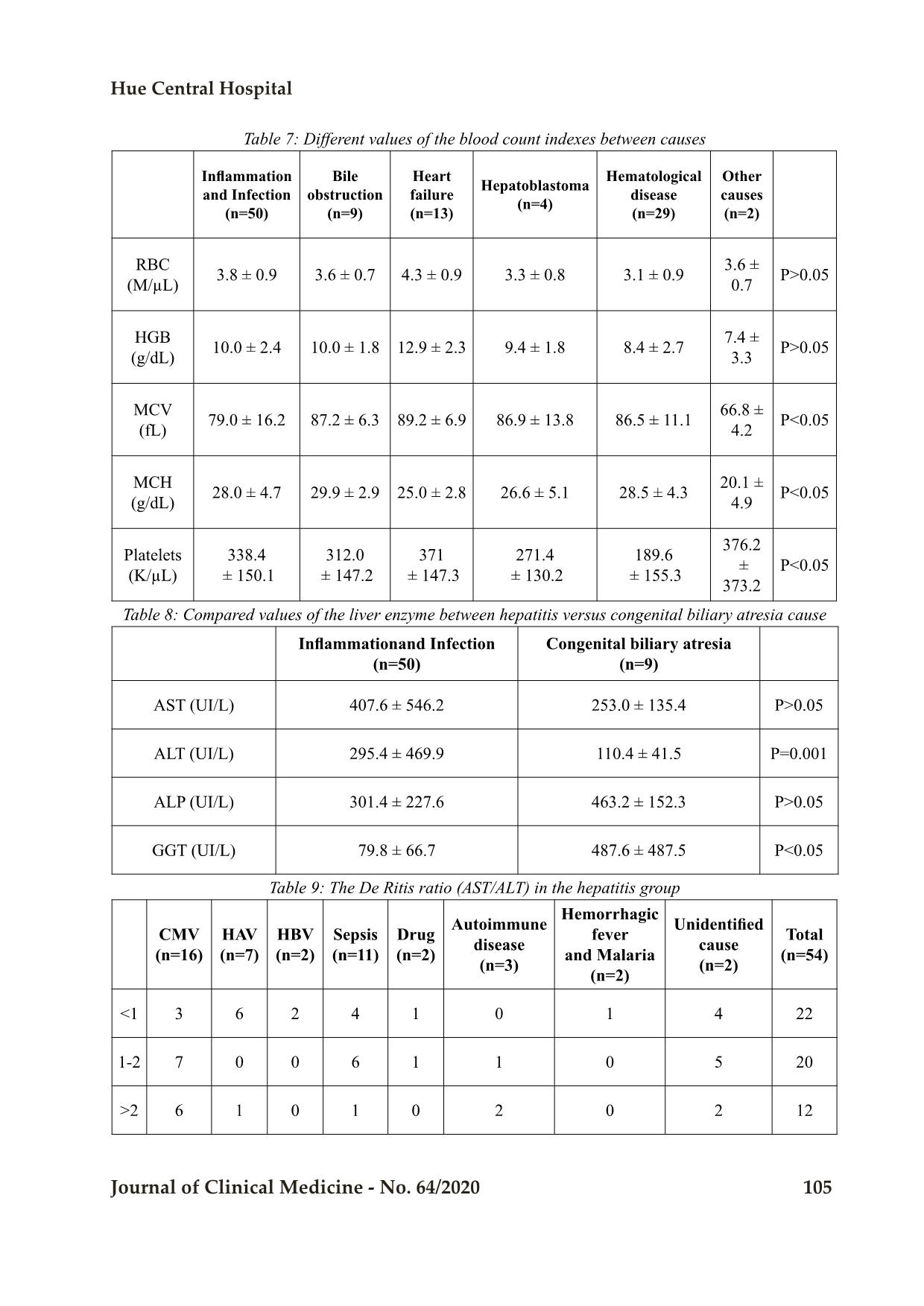
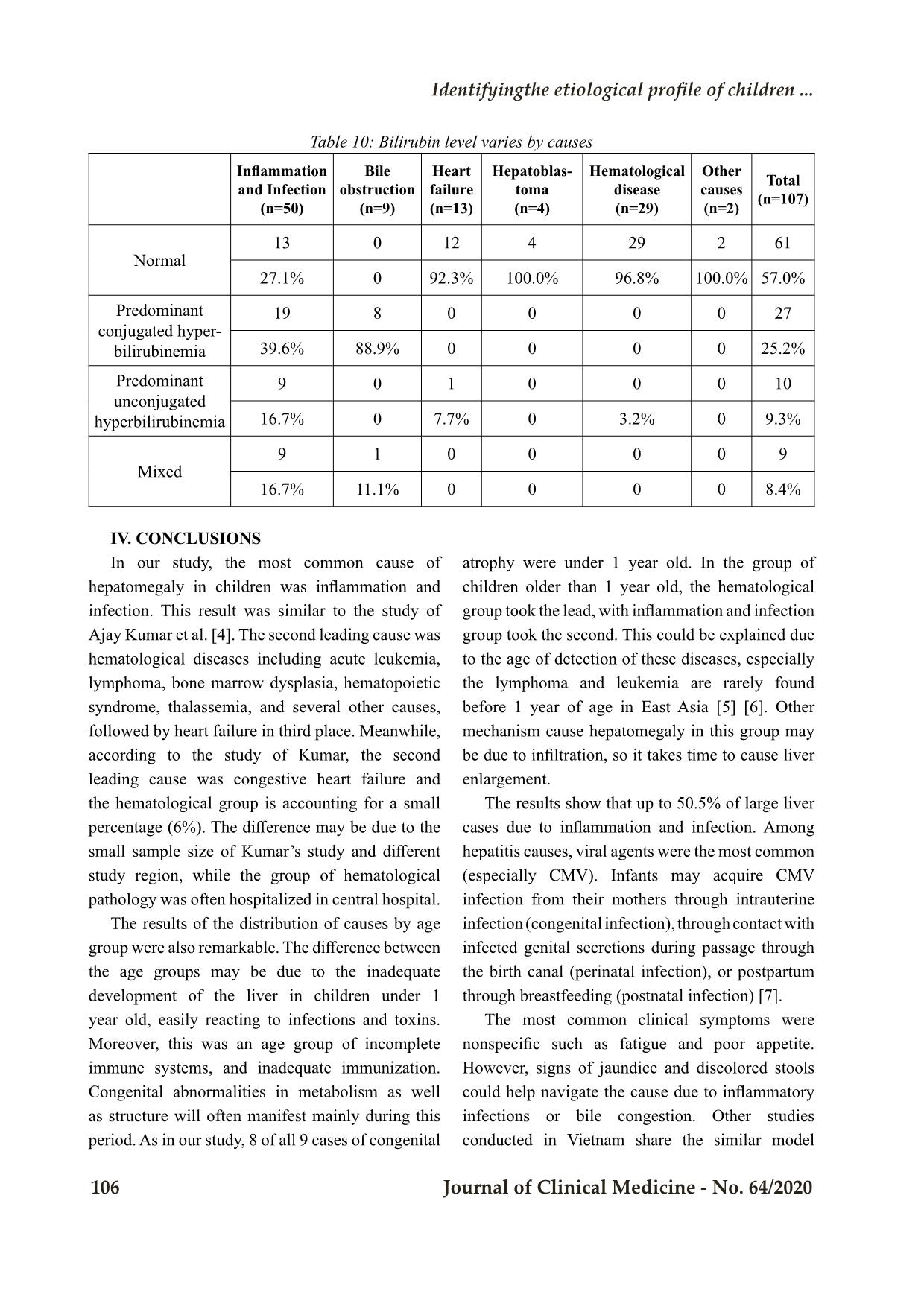
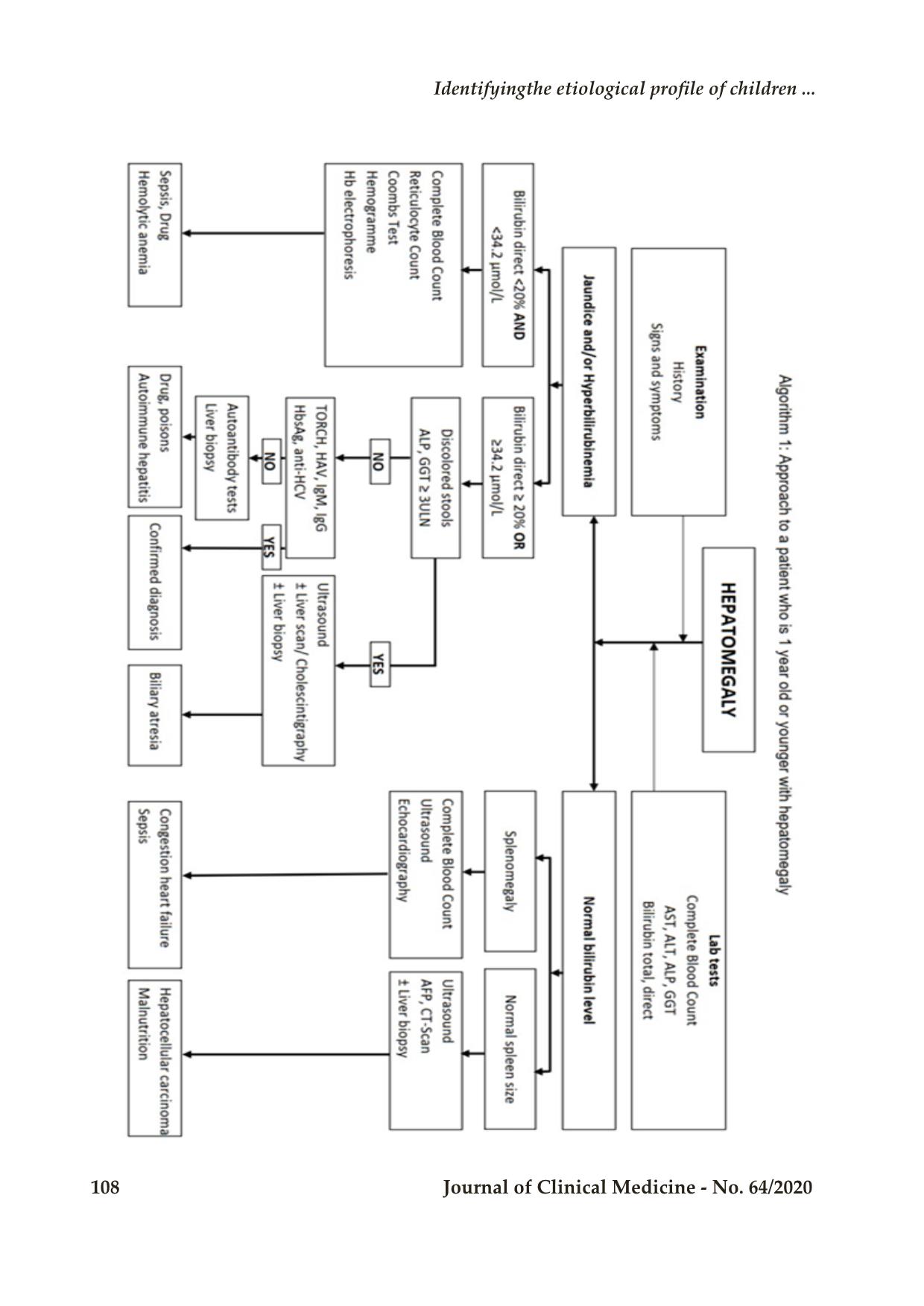
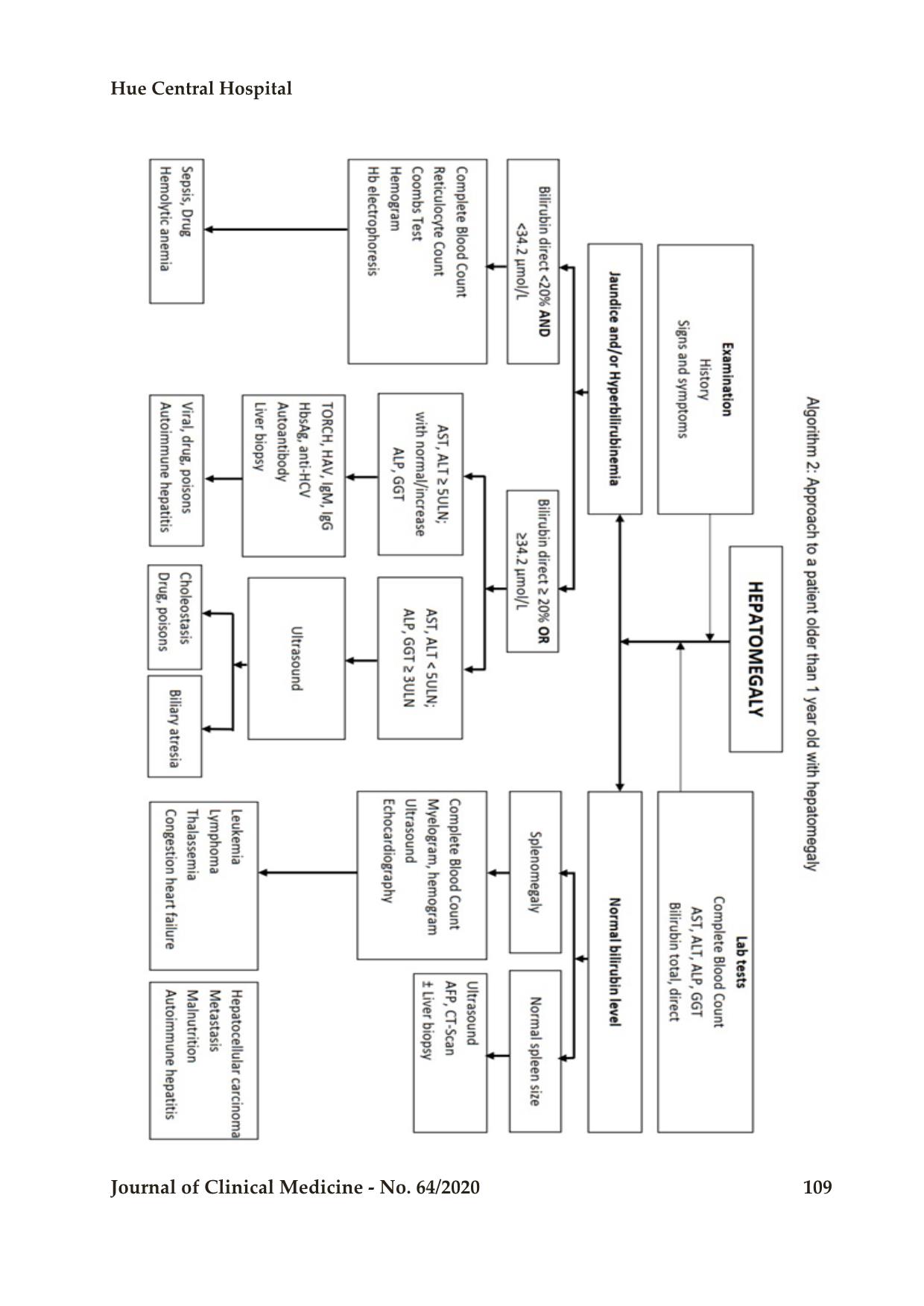
Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 101 Original Research IDENTIFYING THE ETIOLOGICAL PROFILE OF CHILDREN PRESENTED WITH HEPATOMEGALY ADMITTED TO A TERTIARY CARE HOSPITAL Nguyen Khoi Quan1, Nguyen Huu Chau Duc2,3* DOI: 10.38103/jcmhch.2020.64.15 ABSTRACT Objectives: To identify the pattern and etiology of diseases in children presented hepatomegaly at Pediatrics Department in Hue Central Hospital, Vietnam. Material and Methods: The Present study was conducted to evaluate the possible etiology and clinical features of children presented with hepatomegaly. A total of 107 children, from one month to fifteen years of age with hepatomegaly admitted in the Pediatric Department of Hue Central Hospital, Vietnam from May 2018 to April 2019 were included in this study. Results: The most common causes of hepatomegaly were inflammation/infection of the liver (miscellaneous cause included), hematological diseases and congestion heart failure with the percentage of 50.5%; 27,1% and 12,1%; respectively. Among the hepatitis group, viral agents account for nearly 50.0%, of which the most common one was Cytomegalovirus accounting for nearly 30.0%. Distribution of causes by age group revealed most cases in 1 year-old or younger children was caused by inflammation (53.8%), and in the older than 1 year-old children were hematological disorders (47.3%) which has statistical significance (P<0.05). Conclusions: Our research observed that the most common causes of the group of ≤ 1 year old were hepatitis, followed by cardiovascular disease and biliary obstruction due to congenital biliary atresia, and in the older than 1 year group, hematological disorders was the most common. Keywords: hepatomegaly, etiology, hepatitis I. INTRODUCTION Hepatomegaly is an enlargement of the liver. Abnormal liver enlargement is a manifestation of many different causes: liver disease such as hepatitis, biliary obstruction, or it is a sign of systemic causes such as sepsis, blood disease, and heart disease. There are many causes that can be cured, but others can also lead to death, or certain complications if the treatment is not appropriate. On the other hand, the size of the liver in children also varies depending on the age and the development of the body, so it is difficult to determine the abnormal liver enlargement in clinical practice. Treatment of hepatomegaly strongly depends on the pathological mechanisms behind, so accurate diagnosis is crucial. Identification of the mechanism behind an enlarged liver is a challenge, because the patients rarely present with a single symptom, but 1 Faculty of Medicine, Hue University of Medicine and Pharmacy, Hue University 2 Pediatrics Department, Hue University of Medicine and Pharmacy, Hue University 3 Pediatrics Center, Hue Central Hospital - Received: 2/6/2020; Revised: 13/8/2020; - Accepted: 4/9/2020 - Corresponding author: Nguyen Huu Chau Duc - Email: nhcduc@huemed-univ.edu.vn; Phone: 0949902121 Bệnh viện Trung ương Huế 102 Journal of Clinical Medicine - No. 64/2020 often contemporary associated many symptoms. The differences in many causes and their serious effects on children also require early detection and prognosis of the serious risk factors, in order to have an early and appropriate treatment to prevent complications and death. Currently, thanks to modern testing techniques, most causes of hepatomegaly have been discovered, and the disease has been prevented and treated with efficiency. Unfortunately, some laboratory tests are not available in many healthcare facilities. A simple algorithm using a few common parameters with easy-approach is needed in the facilities and also for primary medical care. All over the world as well as in Vietnam, studies about the etiology of hepatomegaly is limited [1]. Most studies focus on one specific cause, separately on each different study subject [2] [3]. In order to contribute to the subject and improve the capacity of diagnosis, we conducted the research with three objectives: to reveal the etiology of hepatomegaly in children; to describe the clinical and laboratory characteristics of hepatomegaly children, and we also present a clinical-approach algorithm to apply into practice. II. MATERIAL AND METHODS A total 107 children from 1 moth to 15 years of age admitted with hepatomegaly into the Pediatric Department of Hue Central Hospital, Vietnam from May 2018 to April 2019 included in the study. Children with incomplete data were excluded from this study. Those children presented with pushed down liver due to various causes are excluded by measuring liver span for that particular age. Hepatomegaly was defined as when the liver edge was palpated below the right costal margin at the mid clavicular line for infants and older children and the liver span should be more than the ex ... ent. Data were collected from register book of the patient by using data entry preform, which was prepared by the researchers themselves. After collection of relevant information the data were checked, verified, edited manually for consistency, accuracy and to reduce error. Statistical analysis was done by statistical software SPSS for windows version 20. P values were calculated using Pearson chi- square test. P < 0.05 was considered as significant and P < 0.01 as highly significant. III. RESULTS Based on the data collected from 107 subjects, the children were divided into two age groups: 1 month to ≤1 year old (called ≤1 year) and > 1 to 15 years old (called >1 year) (Table 2). The proportion of male and female between the two age groups was not statistically significant. 3.1. The etiologies of hepatomegaly in children The causes of hepatomegaly were described in Table 3. Three most common causes of hepatomegaly was inflammation/infection of the liver (miscellaneous causes were included), hematological diseases and congestion heart failure with the percentage of 50.5%; 27,1% and 12,1%; respectively. The miscellaneous cases included were four cases of CMV hepatitis combined with congenital biliary atresia. Table 2: Distribution of disease by age group and sex Male Female Total n % n % n % ≤1 year 28 26.2 24 22.4 52 48.6 P>0.05>1 year 27 25.2 28 26.2 55 51.4 Total 55 51.4 52 48.6 107 100 Identifyingthe etiological profile of children ... Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 103 Table 3: Etiology of hepatomegaly Etiology Number of cases (and percentage) Inflammation and infection 50 (46.8) Bile obstruction 5 (4.7) Heart failure 13 (12.1) Liver cancer 4 (3.7) Hematological disease 29 (27.1) Other rarely causes 2 (1.9) Miscellaneous causes (CMV infection combined with congenital biliary atresia) 4 (3.7) Total 107 (100) With the group of 1 moth to ≤ 1 year old, the three most common cause groups were hepatitis, followed by cardiovascular disease and biliary obstruction due to congenital biliary atresia accounting for 53.8%, 21.2% and 15.4%, respectively. For the group > 1 to year, the most common was the hematological cause, accounting for 47.3%, followed by inflammation and infection 40.0%, the remaining causes include liver cancer, rare biliary atrophy. The difference in the proportion distribution was statistically significant between two age groups (P<0.05) but not significant between two genders. The results in table 4 were shown that among the causes of hepatitis, the viral agent accounts for nearly half of cases, of which the most common was CMV, followed by sepsis and neonatal infection. Some other rare causes such as drugs, autoimmune and other. However, there still 20.4% of cases were unknown etiology. In 54 cases of hepatitis, with the group of ≤1 year old (31 cases), the most common cause of hepatitis was CMV, accounting for 15/31 (48.4%). After that, it was due to urgent infection accounting for 7/31 (22.6%). There still a large proportion of unknown causes was 7/31 (22.6%). For the group > 1 year old, the most common cause of hepatitis was viral 8/23 cases, of which HAV was presented in 6/8 case. The difference in the proportion distribution was statistically significant (P=0.001). Table 4: Distribution of hepatitis causes by age group Hepatitis cause Number of cases ≤1 year old >1 year old CMV 15 1 HAV 1 6 HBV 0 2 Sepsis 7 4 Drug 1 1 Autoimmune hepatitis 0 3 Hemorrhagic fever 0 1 Malaria 0 1 Unidentified causes 7 4 Total 31 23 3.2. Clinical manifestations of the children with hepatomegaly In table 5, the distribution of liver size by causes was also remarkable. The mean sub-hepatic edge compared to the right costal margin was 3.3 ± 1.4 cm. Mean value in the liver cancer group was the largest (5.3 ± 2.6 cm) and the difference between causes was statistically significant (P<0.05). Most causes were presented with a smooth liver surface (94.4%), except for the group of liver cancer with all four cases having a rough surface. Most causes had a solid liver density (86.0%). Liver tenderness was mainly seen in the group of hepatitis, while 36/107 (more than 30%) cases cannot be evaluated and the differences in tenderness were not statistically significant. Bệnh viện Trung ương Huế 104 Journal of Clinical Medicine - No. 64/2020 Table 5: The mean sub-hepatic edge compared to the right costal margin Etiology Mean size of the liver Inflammation and infection 3,0 ± 1,1 Bile obstruction 3,6 ± 0,5 Heart failure 2,9 ± 0,7 Hepatoblastoma 5,3 ± 2,6 Hematological disease 3,5 ± 1,9 Other causes 3,0 ± 1,4 All causes 3,3 ± 1,4 The clinical manifestations distributed by causes were shown in Table 6. Manifestation of splenomegaly, changes in the number or composition of leukocytes were both not statistically significant when distributed by group of causes. Table 6: The clinical manifestations distributed by causes Inflammation and Infection (n=50) Bile obstruction (n=9) Heart failure (n=13) Hepatoblastoma (n=4) Hematological disease (n=29) Other causes (n=2) Total (n=107) n % Fever 20 3 8 0 16 2 49 45.8 Fatigue 30 5 13 4 28 1 81 75.7 Poor appetite 33 6 13 4 28 2 86 80.4 Jaundice 34 9 0 0 0 0 43 40.2 White stool 7 8 0 0 0 0 15 14.0 Dark urine 34 9 0 1 1 0 45 42.1 Vomiting 16 1 4 0 4 0 25 23.4 Abdominal pain 19 2 2 3 9 0 35 32.7 Diarrhea 5 1 1 0 1 0 8 0.1 Shortness of breath 9 0 13 1 3 1 27 25.2 3.3. Laboratory tests differences according to the causes In the children whose hepatomegaly were hematological disorders, 83.9% had an anemia condition attached. Assessing the severity, most causes had a mild to moderate hepatomegaly condition, while in the hematology group, the rate of severe anemia was 38.7%. The difference in the above rates was statistically significant (P<0.05). The study revealed markedly differences in laboratory test results which were shown in Table 7, 8, 9 and 10. Identifyingthe etiological profile of children ... Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 105 Table 7: Different values of the blood count indexes between causes Inflammation and Infection (n=50) Bile obstruction (n=9) Heart failure (n=13) Hepatoblastoma (n=4) Hematological disease (n=29) Other causes (n=2) RBC (M/µL) 3.8 ± 0.9 3.6 ± 0.7 4.3 ± 0.9 3.3 ± 0.8 3.1 ± 0.9 3.6 ± 0.7 P>0.05 HGB (g/dL) 10.0 ± 2.4 10.0 ± 1.8 12.9 ± 2.3 9.4 ± 1.8 8.4 ± 2.7 7.4 ± 3.3 P>0.05 MCV (fL) 79.0 ± 16.2 87.2 ± 6.3 89.2 ± 6.9 86.9 ± 13.8 86.5 ± 11.1 66.8 ± 4.2 P<0.05 MCH (g/dL) 28.0 ± 4.7 29.9 ± 2.9 25.0 ± 2.8 26.6 ± 5.1 28.5 ± 4.3 20.1 ± 4.9 P<0.05 Platelets (K/µL) 338.4 ± 150.1 312.0 ± 147.2 371 ± 147.3 271.4 ± 130.2 189.6 ± 155.3 376.2 ± 373.2 P<0.05 Table 8: Compared values of the liver enzyme between hepatitis versus congenital biliary atresia cause Inflammationand Infection (n=50) Congenital biliary atresia (n=9) AST (UI/L) 407.6 ± 546.2 253.0 ± 135.4 P>0.05 ALT (UI/L) 295.4 ± 469.9 110.4 ± 41.5 P=0.001 ALP (UI/L) 301.4 ± 227.6 463.2 ± 152.3 P>0.05 GGT (UI/L) 79.8 ± 66.7 487.6 ± 487.5 P<0.05 Table 9: The De Ritis ratio (AST/ALT) in the hepatitis group CMV (n=16) HAV (n=7) HBV (n=2) Sepsis (n=11) Drug (n=2) Autoimmune disease (n=3) Hemorrhagic fever and Malaria (n=2) Unidentified cause (n=2) Total (n=54) <1 3 6 2 4 1 0 1 4 22 1-2 7 0 0 6 1 1 0 5 20 >2 6 1 0 1 0 2 0 2 12 Bệnh viện Trung ương Huế 106 Journal of Clinical Medicine - No. 64/2020 Table 10: Bilirubin level varies by causes Inflammation and Infection (n=50) Bile obstruction (n=9) Heart failure (n=13) Hepatoblas- toma (n=4) Hematological disease (n=29) Other causes (n=2) Total (n=107) Normal 13 0 12 4 29 2 61 27.1% 0 92.3% 100.0% 96.8% 100.0% 57.0% Predominant conjugated hyper- bilirubinemia 19 8 0 0 0 0 27 39.6% 88.9% 0 0 0 0 25.2% Predominant unconjugated hyperbilirubinemia 9 0 1 0 0 0 10 16.7% 0 7.7% 0 3.2% 0 9.3% Mixed 9 1 0 0 0 0 9 16.7% 11.1% 0 0 0 0 8.4% IV. CONCLUSIONS In our study, the most common cause of hepatomegaly in children was inflammation and infection. This result was similar to the study of Ajay Kumar et al. [4]. The second leading cause was hematological diseases including acute leukemia, lymphoma, bone marrow dysplasia, hematopoietic syndrome, thalassemia, and several other causes, followed by heart failure in third place. Meanwhile, according to the study of Kumar, the second leading cause was congestive heart failure and the hematological group is accounting for a small percentage (6%). The difference may be due to the small sample size of Kumar’s study and different study region, while the group of hematological pathology was often hospitalized in central hospital. The results of the distribution of causes by age group were also remarkable. The difference between the age groups may be due to the inadequate development of the liver in children under 1 year old, easily reacting to infections and toxins. Moreover, this was an age group of incomplete immune systems, and inadequate immunization. Congenital abnormalities in metabolism as well as structure will often manifest mainly during this period. As in our study, 8 of all 9 cases of congenital atrophy were under 1 year old. In the group of children older than 1 year old, the hematological group took the lead, with inflammation and infection group took the second. This could be explained due to the age of detection of these diseases, especially the lymphoma and leukemia are rarely found before 1 year of age in East Asia [5] [6]. Other mechanism cause hepatomegaly in this group may be due to infiltration, so it takes time to cause liver enlargement. The results show that up to 50.5% of large liver cases due to inflammation and infection. Among hepatitis causes, viral agents were the most common (especially CMV). Infants may acquire CMV infection from their mothers through intrauterine infection (congenital infection), through contact with infected genital secretions during passage through the birth canal (perinatal infection), or postpartum through breastfeeding (postnatal infection) [7]. The most common clinical symptoms were nonspecific such as fatigue and poor appetite. However, signs of jaundice and discolored stools could help navigate the cause due to inflammatory infections or bile congestion. Other studies conducted in Vietnam share the similar model Identifyingthe etiological profile of children ... Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 107 [8] [9]. Dyspnea were also valuable to suggest heart failure as an underlying condition. We had also evaluated accompanying splenomegaly, but differences were not significant. Changes in complete blood count were most common in the hematological group, characterized by a decrease in both erythrocytes and thrombocytes, with an inconsistent sign of leukopenia. The MCV alterations between the groups were remarkable. These signs were consistent with pathogenesis of liver malfunction. Due to the heterogeneousness of tests, this study focused on differences between the inflammation, infection and biliary obstruction group. In the hepatitis group, increasing AST and ALT were dominant than ALP and GGT; while in the bile obstructive condition, in contrast, ALP and GGT were markedly increased. This difference was explained based on the origin of these enzymes. AST, ALT in hepatitis children reflects the destruction of hepatocytes. ALT mainly originated from cytoplasm while AST was highly localized in the mitochondria (80%) and a little in cytoplasm (20%) therefore increasing AST suggests deep and progressive damage. Beside, ALP was synthesized by hepatocytes and bile duct epithelial cells and GGT was found with high concentrations in the cylindrical epithelial cells of the bile duct, it reveals that ALP and GGT were very sensitive tests to detect biliary obstruction. Bilirubin level was normal in most causes. Bilirubin increase was seen in all cases with biliary obstruction and also in a large number of hepatitis. The obstructive group had direct bilirubin dominance, while in the hepatitis group the difference between the causes was not really clear. Our research strengthens the current understanding of the etiology, clinical and laboratory manifestations of hepatomegaly. Based on these insights, we also propose two schemes for approaching the diagnosis of hepatomegaly by two age groups below (algorithm 1, 2). Conflict of interests All the authors have no conflict of interests to declare. REFERENCES 1. P. Song, ĐĐ. Đức, B. Hiền và cộng sự, “Đánh giá bước đầu căn nguyên viêm gan virus ở Việt Nam. Nghiên cứu lâm sàng căn nguyên học viêm gan virus (1992-1996),” Đề tài KY 01-09, 04 1996. 2. CH. Hầu, “Nghiên cứu tình hình nhiễm viêm gan siêu vi A, B và E trong cộng đồng tại huyện Tân Châu tỉnh An Giang,” in Hội nghị khoa học chuyên đề Vi sinh - Dịch tễ - Miễn dịch, Thành phố Hồ Chí Minh, 1996. 3. NV. Nguyên, “Nghiên cứu lâm sàng, cận lâm sàng và nguyên nhân của viêm gan cấp ở trẻ em tại Bệnh viện Nhi Trung Ương,” Luận văn tốt nghiệp thạc sỹ, Đại học Y Hà Nội, 2015. 4. A. Kumar, “Clinico pathological study of hepatomegaly,” International Journal of Medical and Health Research, vol. 2, no. 1, pp. 60-2, 2016. 5. BL Asselin, DG Tubergen, J Hochberg, “Cancer and Benign Tumors,” in Nelson Textbook of Pediatrics, 20th edition, New York, USA, Elsevier, 2016, pp. 2416-80. 6. K. Nakata, Y. Ito, W. Magadi et al, “Childhood cancer incidence and survival in Japan and England: A population‐based study (1993‐2010),” Cancer Science, vol. 109, no. 2, 2017. 7. MY Hasosah, SY Kutbi, AW Al-Amri et al, “Perinatal cytomegalovirus hepatitis in Saudi infants: a case series,” Saudi J Gastroenterol, vol. 18, pp. 208-13, 2012. 8. [8] PN. An và cộng sự, “Đặc điểm lâm sàng, cận lâm sàng, dịch tễ học và diễn biến của viêm gan virus cấp ở trẻ em trong 5 năm 1991-1995 tại Viện Nhi Trung Ương,” Nhi khoa 7(1), pp. 12-9, 1998. 9. VTH. Yến, “Tìm hiểu căn nguyên, đặc điểm lâm sàng và biến đổi một số chỉ số huyết học, hoá sinh trong viêm gan virus cấp trẻ em tại Bệnh viện Nhi Trung Ương,” Luận văn tốt nghiệp thạc sĩ, Đại học Y Hà Nội, 2003. Bệnh viện Trung ương Huế 108 Journal of Clinical Medicine - No. 64/2020 Identifyingthe etiological profile of children ... Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 109
File đính kèm:
 dentifying_the_etiological_profile_of_children_presented_wit.pdf
dentifying_the_etiological_profile_of_children_presented_wit.pdf

