Castleman disease in children: Diagnosis and treatment
Background: We describe the experiences in diagnosis and results of treatment in pediatric Castleman
disease.
Method: Serial case reports.
Result: From 2016 to 2019, we had 7 cases of pediatric Castleman disease: 3 boys and 4 girl. The
median age at diagnosis was 147 months (121-173 months). Clinical manifestations were found in five
cases. They were all unicentric Castleman disease (6 abdominal mass, one left infraclavicular mass). All
patients were operated with postoperative period uneventful. The median time of postoperative follow up
was 22.7 months (11-53 months) with no signs of relapse.
Conclusions: Pediatric Castleman disease is a rare benign lymph node hyperplasia, it can be localised
or disseminated. Operation is the treatment of choice for localised Castleman disease.
Key words: Castleman disease, angiofollicular lymph node hyperplasia, giant lymph node hyperplasia,
lymph node hamartoma.
Trang 1
Trang 2
Trang 3

Trang 4
Trang 5
Trang 6
Tóm tắt nội dung tài liệu: Castleman disease in children: Diagnosis and treatment

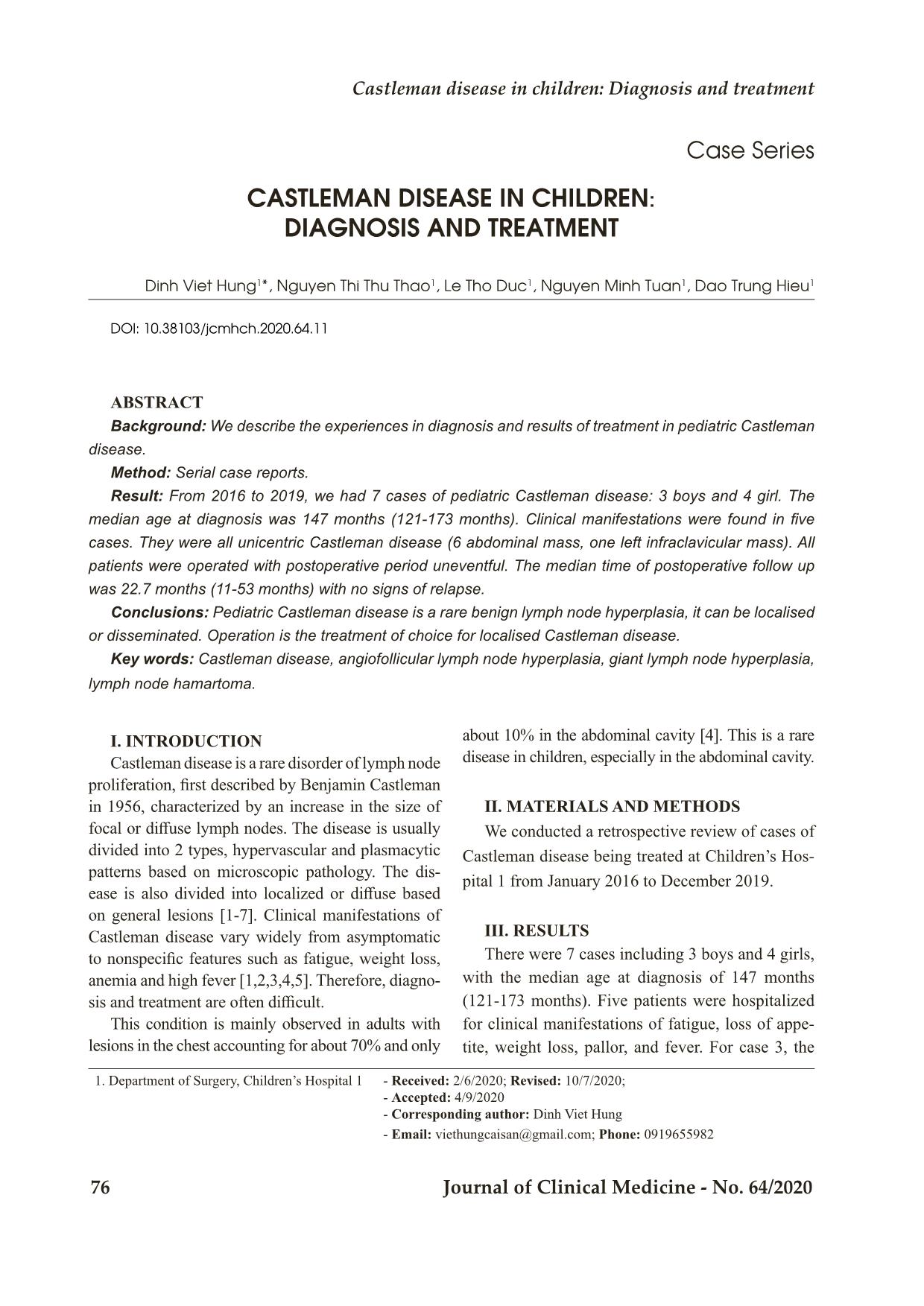
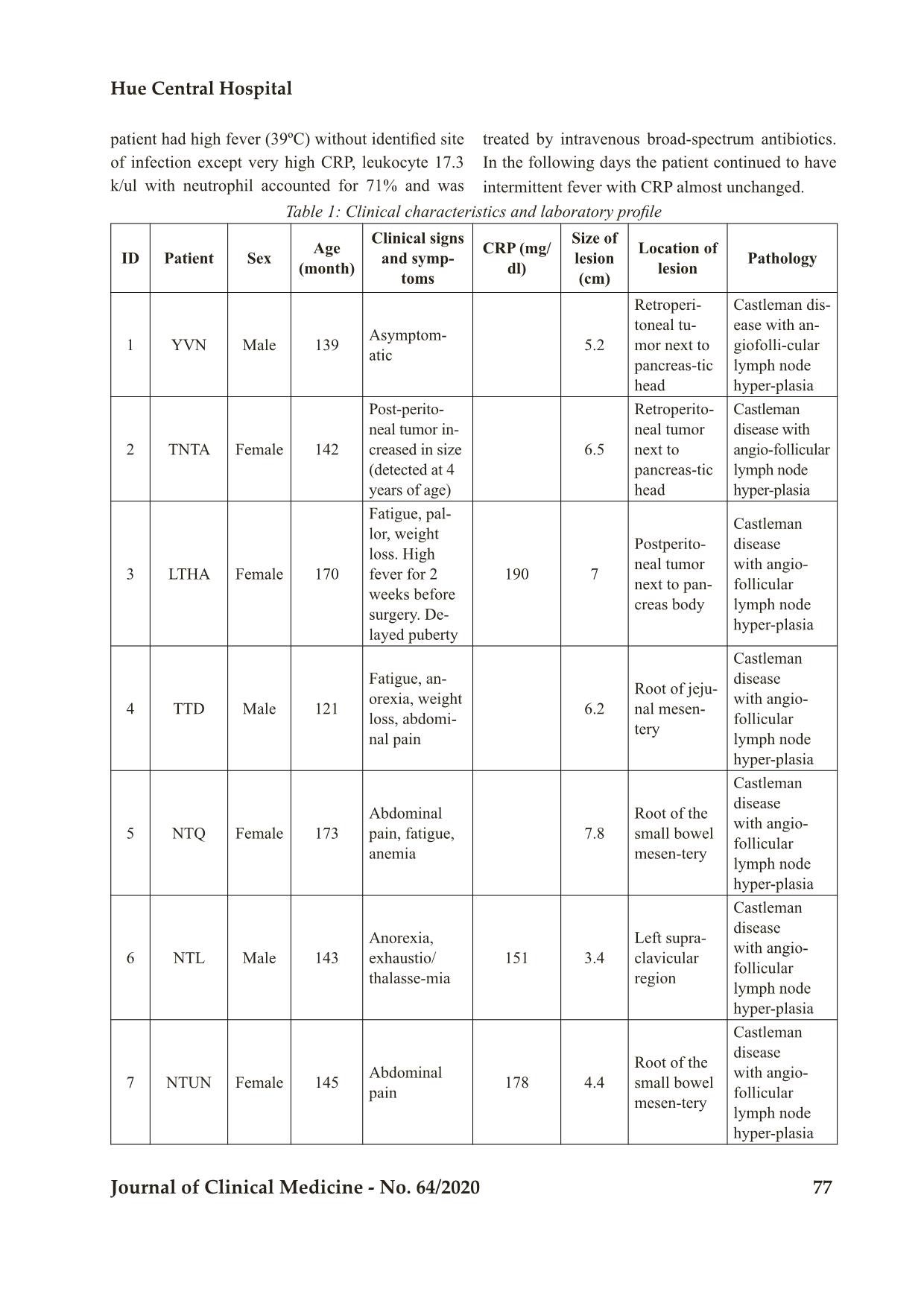
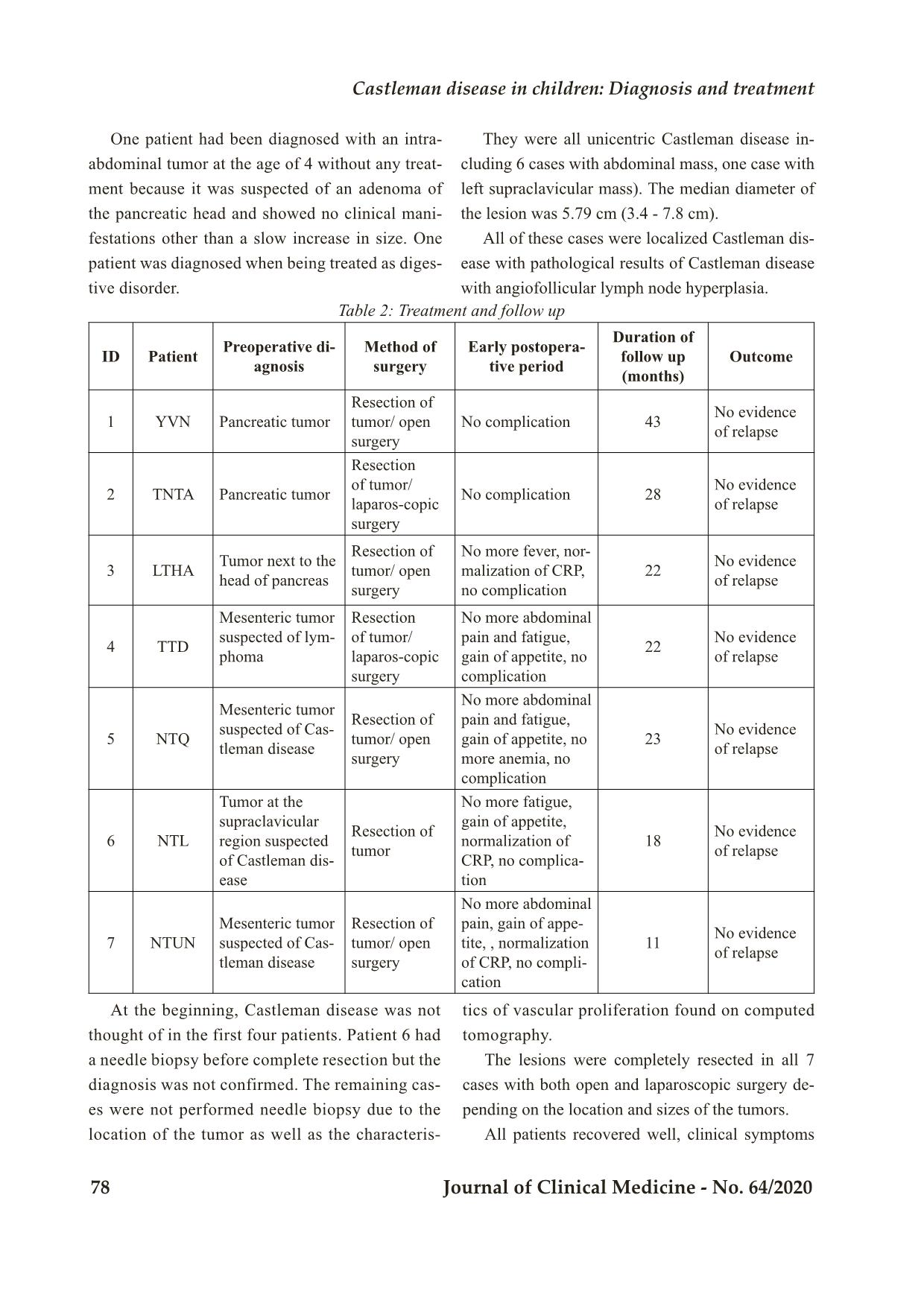
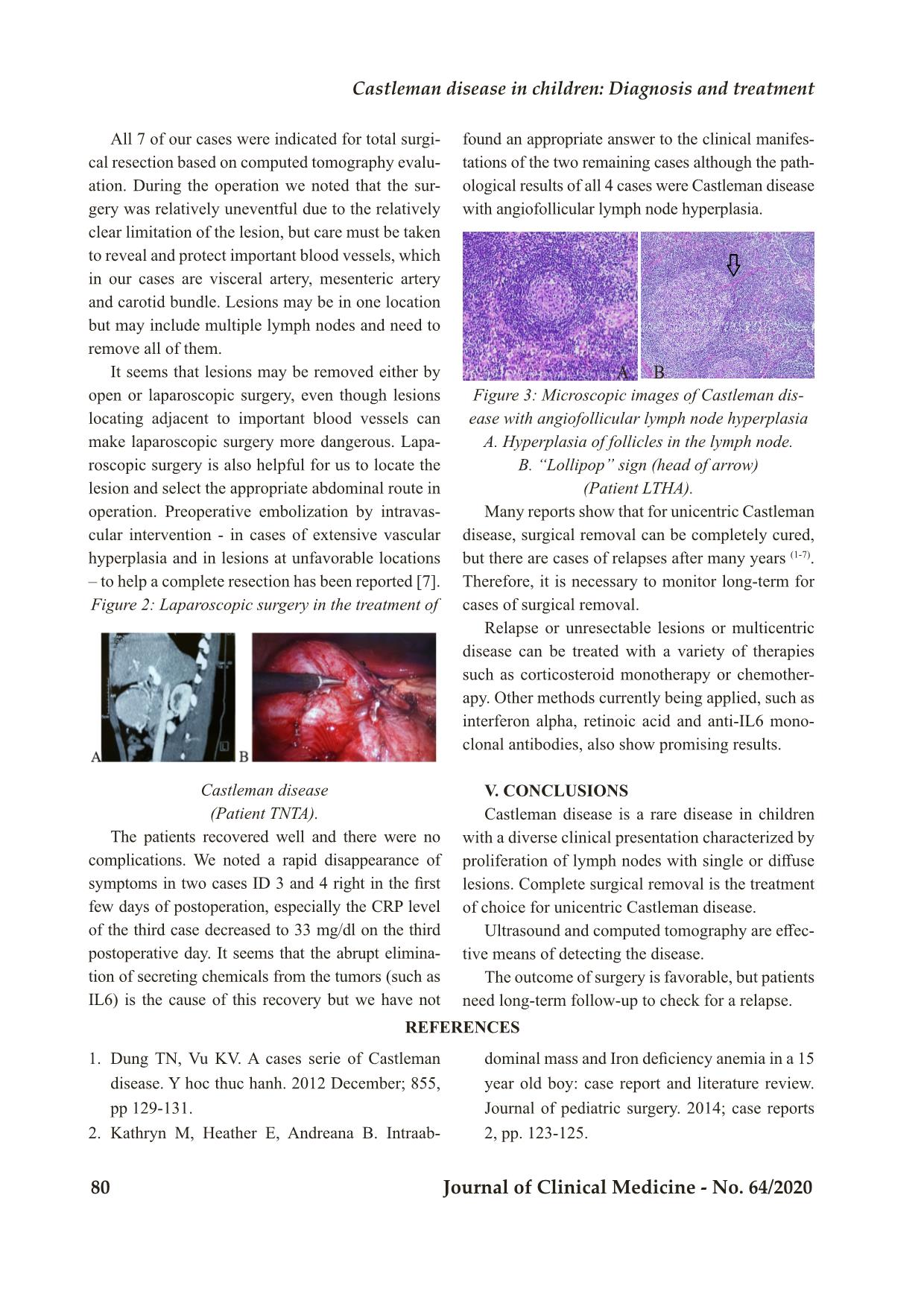
Bệnh viện Trung ương Huế 76 Journal of Clinical Medicine - No. 64/2020 Case Series CASTLEMAN DISEASE IN CHILDREN: DIAGNOSIS AND TREATMENT Dinh Viet Hung1*, Nguyen Thi Thu Thao1, Le Tho Duc1, Nguyen Minh Tuan1, Dao Trung Hieu1 DOI: 10.38103/jcmhch.2020.64.11 ABSTRACT Background: We describe the experiences in diagnosis and results of treatment in pediatric Castleman disease. Method: Serial case reports. Result: From 2016 to 2019, we had 7 cases of pediatric Castleman disease: 3 boys and 4 girl. The median age at diagnosis was 147 months (121-173 months). Clinical manifestations were found in five cases. They were all unicentric Castleman disease (6 abdominal mass, one left infraclavicular mass). All patients were operated with postoperative period uneventful. The median time of postoperative follow up was 22.7 months (11-53 months) with no signs of relapse. Conclusions: Pediatric Castleman disease is a rare benign lymph node hyperplasia, it can be localised or disseminated. Operation is the treatment of choice for localised Castleman disease. Key words: Castleman disease, angiofollicular lymph node hyperplasia, giant lymph node hyperplasia, lymph node hamartoma. 1. Department of Surgery, Children’s Hospital 1 - Received: 2/6/2020; Revised: 10/7/2020; - Accepted: 4/9/2020 - Corresponding author: Dinh Viet Hung - Email: viethungcaisan@gmail.com; Phone: 0919655982 I. INTRODUCTION Castleman disease is a rare disorder of lymph node proliferation, first described by Benjamin Castleman in 1956, characterized by an increase in the size of focal or diffuse lymph nodes. The disease is usually divided into 2 types, hypervascular and plasmacytic patterns based on microscopic pathology. The dis- ease is also divided into localized or diffuse based on general lesions [1-7]. Clinical manifestations of Castleman disease vary widely from asymptomatic to nonspecific features such as fatigue, weight loss, anemia and high fever [1,2,3,4,5]. Therefore, diagno- sis and treatment are often difficult. This condition is mainly observed in adults with lesions in the chest accounting for about 70% and only about 10% in the abdominal cavity [4]. This is a rare disease in children, especially in the abdominal cavity. II. MATERIALS AND METHODS We conducted a retrospective review of cases of Castleman disease being treated at Children’s Hos- pital 1 from January 2016 to December 2019. III. RESULTS There were 7 cases including 3 boys and 4 girls, with the median age at diagnosis of 147 months (121-173 months). Five patients were hospitalized for clinical manifestations of fatigue, loss of appe- tite, weight loss, pallor, and fever. For case 3, the Castleman disease in children: Diagnosis and treatment Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 77 Table 1: Clinical characteristics and laboratory profile ID Patient Sex Age (month) Clinical signs and symp- toms CRP (mg/ dl) Size of lesion (cm) Location of lesion Pathology 1 YVN Male 139 Asymptom-atic 5.2 Retroperi- toneal tu- mor next to pancreas-tic head Castleman dis- ease with an- giofolli-cular lymph node hyper-plasia 2 TNTA Female 142 Post-perito- neal tumor in- creased in size (detected at 4 years of age) 6.5 Retroperito- neal tumor next to pancreas-tic head Castleman disease with angio-follicular lymph node hyper-plasia 3 LTHA Female 170 Fatigue, pal- lor, weight loss. High fever for 2 weeks before surgery. De- layed puberty 190 7 Postperito- neal tumor next to pan- creas body Castleman disease with angio- follicular lymph node hyper-plasia 4 TTD Male 121 Fatigue, an- orexia, weight loss, abdomi- nal pain 6.2 Root of jeju- nal mesen- tery Castleman disease with angio- follicular lymph node hyper-plasia 5 NTQ Female 173 Abdominal pain, fatigue, anemia 7.8 Root of the small bowel mesen-tery Castleman disease with angio- follicular lymph node hyper-plasia 6 NTL Male 143 Anorexia, exhaustio/ thalasse-mia 151 3.4 Left supra- clavicular region Castleman disease with angio- follicular lymph node hyper-plasia 7 NTUN Female 145 Abdominal pain 178 4.4 Root of the small bowel mesen-tery Castleman disease with angio- follicular lymph node hyper-plasia patient had high fever (39ºC) without identified site of infection except very high CRP, leukocyte 17.3 k/ul with neutrophil accounted for 71% and was treated by intravenous broad-spectrum antibiotics. In the following days the patient continued to have intermittent fever with CRP almost unchanged. Bệnh viện Trung ương Huế 78 Journal of Clinical Medicine - No. 64/2020 Table 2: Treatment and follow up ID Patient Preoperative di-agnosis Method of surgery Early postopera- tive period Duration of follow up (months) Outcome 1 YVN Pancreatic tumor Resection of tumor/ open surgery No complication 43 No evidence of relapse 2 TNTA Pancreatic tumor Resection of tumor/ laparos-copic surgery No complication 28 No evidence of relapse 3 LTHA Tumor next to the head of pancreas Resection of tumor/ open surgery No more fever, nor- malization of CRP, no complication 22 No evidence of relapse 4 TTD Mesenteric tumor suspected of lym- phoma Resection of tumor/ laparos-copic surgery No more abdominal pain and fatigue, gain of appetite, no complication 22 No evidence of relapse 5 NTQ Mesenteric tumor suspected of Cas- tleman disease Resection of tumor/ open surgery No more abdominal pain and fatigue, gain of appetite, no more anemia, no complication 23 No evidence of relapse 6 NTL Tumor at the supraclavicular region suspected of Castleman dis- ease Resection of tumor No more fatigue, gain of appetite, normalization of CRP, no complica- tion 18 No evidence of relapse 7 NTUN Mesenteric tumor suspected of Cas- tleman disease Resection of tumor/ open surgery No more abdominal pain, gain of appe- tite, , normalization of CRP, no compli- cation 11 No evidence of relapse One patient had been diagnosed with an intra- abdominal tumor at the age of 4 without any treat- ment because it was suspected of an adenoma of the pancreatic head and showed no clinical mani- festations other than a slow increase in size. One patient was diagnosed when being treated as diges- tive disorder. They were all unicentric Castleman disease in- cluding 6 cases with abdominal mass, one case with left supraclavicular mass). The median diameter of the lesion was 5.79 cm (3.4 - 7.8 cm). All of these cases were localized Castleman dis- ease with pathological results of Castleman disease with angiofollicular lymph node hyperplasia. At the beginning, Castleman disease was not thought of in the first four patients. Patient 6 had a needle biopsy before complete resection but the diagnosis was not confirmed. The remaining cas- es were not performed needle biopsy due to the location of the tumor as well as the characteris- tics of vascular proliferation found on computed tomography. The lesions were completely resected in all 7 cases with both open and laparoscopic surgery de- pending on the location and sizes of the tumors. All patients recovered well, clinical symptoms Castleman disease in children: Diagnosis and treatment Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 79 quickly disappeared right in the first few days after surgery. Antibiotics for cases with fever were dis- continued as soon as the results of pathological find- ings were obtained and CRP levels decreased to 33 mg/dl on the third postoperative day. These patients were discharged and monitored based on clinical manifestations and periodic ul- trasound examination with a median follow-up time of 22.7 months (11-53 months). Results at follow-up showed a physical recovery, gain of ap- petite as well as the disappearance of symptoms and no signs of relapse. IV. DISCUSSION Castleman disease is a benign proliferation of lymphocytes and cytoplasm, also known by other names: giant lymph node hyperplasia, lymph node hamartoma, angiofollicular lymph node hyperplasia [4]. Since the first case with lesions locating in the an- terior mediastinum in adults was described by Cas- tleman et al in 1954, an increasing number of cases have been reported with various locations of the lym- phatic system. Castleman disease appears to occur in any location of the body’s lymphatic system, with the most common site being the anterior mediastinum accounting for about 70%, only less than 10% in the abdominal cavity followed by the neck [2,4]. Six out of 7 cases in our report had intra-ab- dominal lesions, perhaps a coincidence to help us learn from the diagnosis and treatment of this rare disease. However, we believe that many cases of Castleman disease in the mediastinum as well as many other sites have not been detected due to the absence of clinical manifestations such as the case of patient 2 showing that this disease can progress silently asymptomatic for years. Although the pathogenesis is still poorly un- derstood, several reports have noted an association between clinical manifestations and an increase in Interleukin 6 [2]. Clinically, the multicentric Castle- man disease with mainly cytoplasmic pattern in mi- croscopic examination often presents with systemic symptoms such as enlargement of lymph nodes, fever, fatigue, weight loss, autoimmune disorders, recurrent infections, anemia, hypoalbuminemia, in- creased CRP, etc [4,6,7]. Five out of seven cases in our report showed symptoms despite the pathological results being angiofollicular lymph node hyperplasia. Previous reports have not shown an association of tumor size with clinical symptoms. In order to diagnose Castleman disease, diagnos- tic imaging tests such as ultrasound or chest and ab- domen CT scans are recommended for patients with symptoms such as fatigue, loss of appetite, anemia, prolonged fever but not yet found the cause. Screen- ing ultrasound during routine physical exams is rec- ommended to detect lesions without clinical mani- festations. Until now, surgical removal of the entire lesion is the first-choice method for the treatment of unicentric Castleman disease. The disease is treated right after diagnosis, although no studies have shown the ability and time for the unicentric disease to turn into multi- centric disease, but the risk of progression to malig- nancy (lymphoma) has been reported [1,3,5]. The proliferation of blood vessels of the lesion [7] makes needle biopsy dangerous. On the other hand, the biopsy results obtained are also very difficult for definitive diagnosis. Therefore, surgical removal of the entire lesion is usually performed without prior pathological diagnosis. Figure 1: Open surgery to treat Castleman disease (A,B: Lesions on CT scan and during surgery; C: Lesion from complete resection of the tumor) (Patient LTHA). Bệnh viện Trung ương Huế 80 Journal of Clinical Medicine - No. 64/2020 All 7 of our cases were indicated for total surgi- cal resection based on computed tomography evalu- ation. During the operation we noted that the sur- gery was relatively uneventful due to the relatively clear limitation of the lesion, but care must be taken to reveal and protect important blood vessels, which in our cases are visceral artery, mesenteric artery and carotid bundle. Lesions may be in one location but may include multiple lymph nodes and need to remove all of them. It seems that lesions may be removed either by open or laparoscopic surgery, even though lesions locating adjacent to important blood vessels can make laparoscopic surgery more dangerous. Lapa- roscopic surgery is also helpful for us to locate the lesion and select the appropriate abdominal route in operation. Preoperative embolization by intravas- cular intervention - in cases of extensive vascular hyperplasia and in lesions at unfavorable locations – to help a complete resection has been reported [7]. Figure 2: Laparoscopic surgery in the treatment of found an appropriate answer to the clinical manifes- tations of the two remaining cases although the path- ological results of all 4 cases were Castleman disease with angiofollicular lymph node hyperplasia. Figure 3: Microscopic images of Castleman dis- ease with angiofollicular lymph node hyperplasia A. Hyperplasia of follicles in the lymph node. B. “Lollipop” sign (head of arrow) (Patient LTHA). Many reports show that for unicentric Castleman disease, surgical removal can be completely cured, but there are cases of relapses after many years (1-7). Therefore, it is necessary to monitor long-term for cases of surgical removal. Relapse or unresectable lesions or multicentric disease can be treated with a variety of therapies such as corticosteroid monotherapy or chemother- apy. Other methods currently being applied, such as interferon alpha, retinoic acid and anti-IL6 mono- clonal antibodies, also show promising results. V. CONCLUSIONS Castleman disease is a rare disease in children with a diverse clinical presentation characterized by proliferation of lymph nodes with single or diffuse lesions. Complete surgical removal is the treatment of choice for unicentric Castleman disease. Ultrasound and computed tomography are effec- tive means of detecting the disease. The outcome of surgery is favorable, but patients need long-term follow-up to check for a relapse. Castleman disease (Patient TNTA). The patients recovered well and there were no complications. We noted a rapid disappearance of symptoms in two cases ID 3 and 4 right in the first few days of postoperation, especially the CRP level of the third case decreased to 33 mg/dl on the third postoperative day. It seems that the abrupt elimina- tion of secreting chemicals from the tumors (such as IL6) is the cause of this recovery but we have not A B REFERENCES 1. Dung TN, Vu KV. A cases serie of Castleman disease. Y hoc thuc hanh. 2012 December; 855, pp 129-131. 2. Kathryn M, Heather E, Andreana B. Intraab- dominal mass and Iron deficiency anemia in a 15 year old boy: case report and literature review. Journal of pediatric surgery. 2014; case reports 2, pp. 123-125. Castleman disease in children: Diagnosis and treatment Hue Central Hospital Journal of Clinical Medicine - No. 64/2020 81 3. Keely B, Deborah P, Christine R, Shahab A. Castleman disease: surgical cure in pediatric pa- tients. Journal of pediatric surgery. 2009. 44, pp. E5-E8. 4. Ke RZ, Hui MJ(2008). Mesenteric castleman disease. Journal of pediatric surgery.2008; 44, pp.1398-1400. 5. Idil RU, Zuhal A, Ibrahim K. Castleman dis- ease: an usual diagnosis of a portal mass in an 8 year old boy. Journal of pediatric surgery, 2010; 46, pp. E9-E11. 6. Jan FS, Mats MH, et al. Minimal access surgery in cactleman disease in a child, a case report. Journal of pediatric surgery.2015; case reports 3, pp. 289-291. 7. Shawn DS, Anand SL, Samuel AM. Preop- erative embolization as an adjunct to the op- erative management of mediastinal castleman disease. Journal of pediatric surgery. 2003; 38 No9, pp. E43.
File đính kèm:
 castleman_disease_in_children_diagnosis_and_treatment.pdf
castleman_disease_in_children_diagnosis_and_treatment.pdf

